I am planning to work in collaboration with the local healthcare workers at Arusha Lutheran Medical Center and Selian Lutheran Hospital in Arusha, Tanzania to address asthma education and medication accessibility. Our goal is to identify barriers to asthma medication, and find ways to alleviate those barriers such that patients can access the medications they need. Specifically, we will focus on the available asthma medications in individual pharmacies in Arusha, Tanzania, identify price, availability, distance needed to travel to obtain medication, and educate about asthma. In doing so, ideally we will then be able to alleviate those barriers and/or anticipate how these barriers affect our patients when prescribing asthma medications. By raising awareness and doing a thorough and holistic examination of asthma supply and accessibility, we hope to then impact the specific medications that are prescribed- for example, if a specific LABA is more widely available than others, to encourage providers to prescribe that medication. Ultimately, the goal will be to increase accessibility, thereby improving outpatient management of asthma and decreasing hospitalizations due to asthma exacerbations.
We also plan to work on educational asthma lectures and pamphlets for patients and for providers if that is something the local healthcare workers find useful; this project had initially gained momentum prior to the COVID-19 pandemic and at that time, feedback from the community was positive. The educational lectures would be given to the Tanzanian interns/residents and would include the latest GINA guidelines, technique on asthma inhaler use with spacers, and would also include a handout component. We hope to use the guidelines and the knowledge we acquire regarding medication accessibility to create guidelines and protocols specific to the Tanzanian healthcare system- both inpatient and outpatient- for asthma treatment.
We hope that children and families impacted by asthma, as well as healthcare workers who care for children with asthma, will benefit from this project. Asthma affects a large proportion of the pediatric population and asthma-related hospitalizations and deaths can be prevented with appropriate education and medications. However, social determinants of health greatly impact accessibility to healthcare and long-term health outcomes, and should be acknowledged when providing healthcare. As physicians, we should do our best to minimize barriers to care for our patients. While many regions would benefit from asthma education and resources, Tanzania has higher rates of asthma/wheezing than many other parts of the world.
Arusha is a more urban setting, and studies have shown that urban areas of Tanzania have higher rates of wheezing and severe asthma attacks compared to rural areas. Furthermore, the overall death rate from asthma is higher in Africa than it is in North and South America, as well as Eastern Asia, Australia, and Europe. Asthma is in the top 30 causes of death in Tanzania, with a rate of 7.03 per 100,000 based off the latest WHO data. This is more than seven-fold the US death rate for asthma- 0.83 per 100,000. Additionally, there have been some reports about the cultural norms surrounding asthma in Tanzania that suggest some of the population worries it is contagious, which could contribute to stigmatization.
We hope that education surrounding asthma could help encourage patients to seek and adhere to asthma treatment. We also hope that by working in collaboration with the Tanzanian healthcare workers, we can foster a bidirectional exchange of knowledge which leads to more informed practices for both Tanzanian and US physicians.
I expect that our focus on barriers to care will shed light on the accessibility issues facing children with asthma. Ideally, our project will pinpoint which medications are accessible and which ones aren’t, based on cost, availability, method of use (inhaler vs inhaler with spacer vs nebulizers). In doing so, we should then be able to knowledgably work within those parameters and prescribe medications that the patients can more easily access and use, thus reducing exacerbations and hospitalizations. I also expect that our education will have a long-lasting impact; by educating healthcare workers, they will be able to continue with that education long after we have left Tanzania. We should also be able to develop inpatient and outpatient protocols based on the knowledge we acquire that is specific to Arusha, and factors in the barriers to care that this population faces in particular, which can be used and adapted for years after our departure.











The sun streamed through the windows as I sat in a sea of white coats. I had dreamed of a moment like this for what seemed like forever. I remember being a 5 year old, sitting at Dr. Jody’s office and saying I wanted to be a doctor when I grew up. 23 years later, and here I was, halfway across the world.
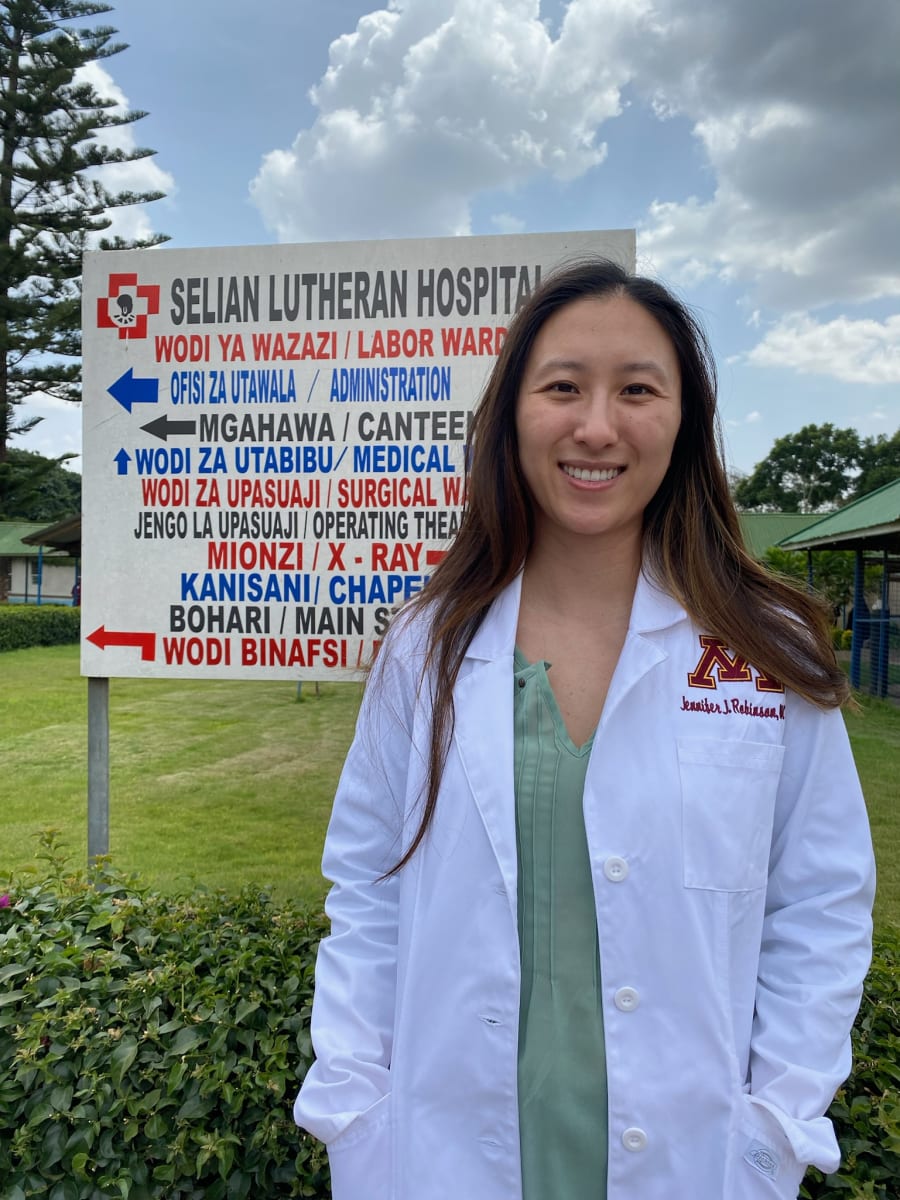
While in Tanzania, I had the opportunity to work at two different hospitals, and a clinic that addressed general pediatric health concerns as well as pre-op evaluations for patients with cleft lips, fluorosis, etc. I was also able to do a rural clinic near Tarangire National Park. Throughout my time there, I saw a myriad of conditions that I had not seen in the United States and that were very impactful to my education as a resident physician.
I saw and treated many conditions that I also see in the United States, including asthma. February is one of the hottest months of the year in Arusha, and is quite dusty. While asthma exacerbations are not rare there, sometimes diagnosing asthma can be difficult. I was able to visit many of the main pharmacies in the city and identify what asthma medications were available. We are planning to use this information to develop further guidelines in collaboration with the Tanzanian doctors for the treatment of asthma.
Although I’ll remember the asthma project, the cases I saw, and the view of Mt. Meru from my apartment, I think what I’ll remember the most are the people. I’ll remember the mother of a patient who had a seizure, and the way all I could do was put my hand on her shoulder, but despite the language barrier it seemed like we had an understanding. I’ll remember the kind, Tanzanian, Masaii woman who was a cancer survivor and a physician. I’ll remember my driver who’d had a life-saving procedure from a foreign doctor when he was a baby, so was named after that. I’ll remember standing on the steps of the hospital as we talked about celebrating women’s day, and the pride I felt as a first generation doctor and immigrant to stand among such incredible women physicians.
This trip reminded me some of the reasons why I wanted to become a doctor in the first place. It brought a new perspective to my work, and I am incredibly grateful to the Doximity foundation for making it possible.