Infant respiratory distress is a leading cause of under-5 mortality worldwide, leading to over one million infant deaths every year with 99% of these deaths in low to middle income countries. Conventional ventilation equipment costs $10,000+ and requires continuous electricity and highly trained operators, leaving infants in resource-constrained settings without access to life saving treatment.
By training local physicians in nurses in the implementation of bubble NIPPV (Non-Invasive Positive Pressure Ventilation), we seek to provide clinicians in resource-constrained settings with additional tools for management of infants with respiratory distress. The focus of this trip will be on training physicians and nurses in the use of this low-cost, low-tech means of respiratory support.
Neonates in respiratory distress without contraindications to noninvasive positive pressure ventilation in Arusha, Tanzania.
This hospital serves as a regional training hub for nurses and physicians caring for neonates, so any NIPPV training delivered here has the potential to impact many more infants in the region.
The University of Minnesota Department of Pediatrics has a longitudinal relationship with this hospital with bi-directional transfer of trainees. This hospital has a well set up Neonatal Intensive Care Unit with qualified nurses and physicians who have already started implementing Non Invasive Positive Pressure Ventilation. In addition, this center is a regional training hub, so any NIPPV training delivered here has the potential to impact many more infants in the region.
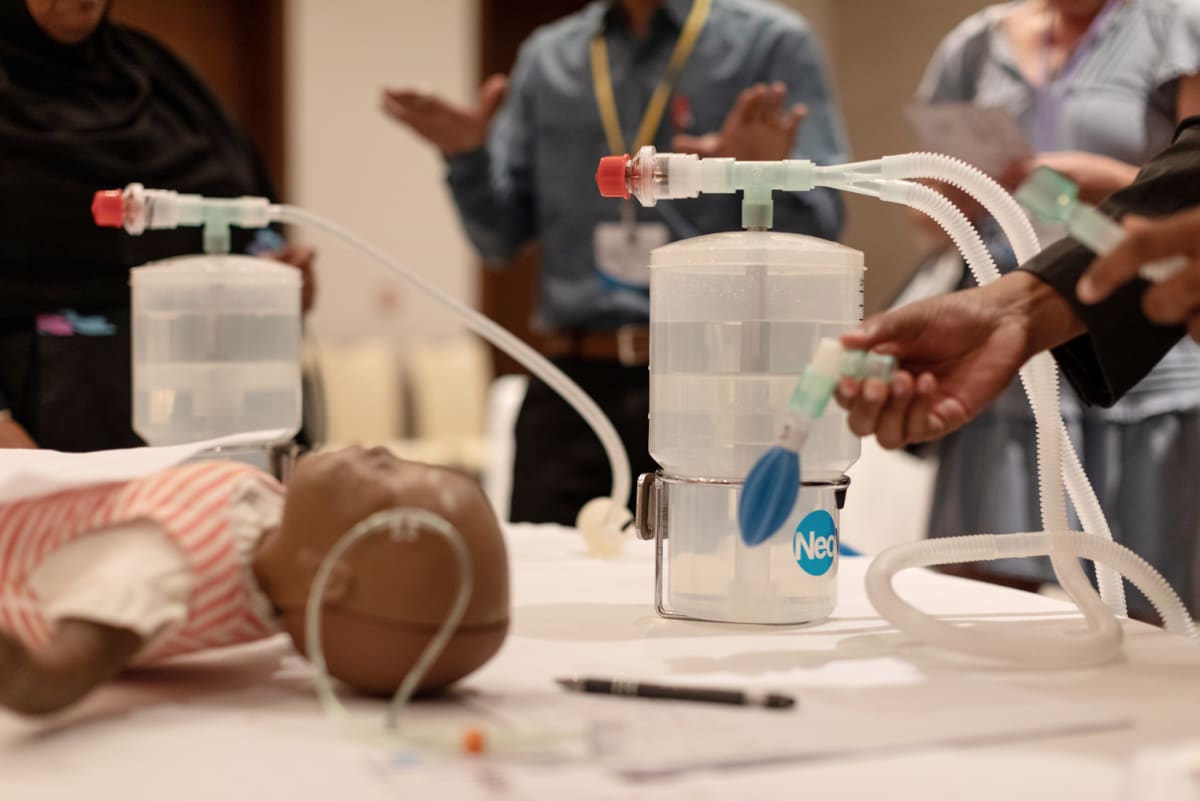





Neonatology Africa’s 4th annual “Tiny Feet, Big Steps” conference was an intensive week of sharing knowledge, experience, and skills to help babies thrive in low-resource settings across Africa. It was an honor to be a part of this conference and interact with the 200+ physicians and nurses caring for infants in low-resource settings.