In a culture where expressing your emotions and feelings is deemed a sign of weakness, getting the help you need for your mental health is impossible. Growing up in Ghana, I was taught to keep my emotions to myself, not speak of my mental well-being, and pray about my struggles; handling your battles alone and in private shows how strong you are. This idea of expression as a sign of weakness transcends the African continent and cultures abroad, including major cities in the US, such as New York. The lack of understanding that one's thoughts and emotions can significantly impact one's physical health drives the misconception that mental illness is not a disease process.
I saw people beaten, outcast, and maltreated in the same culture because of their mental health. Instead of receiving care, these people were called "mad people." As a child, I knew something wasn't right. I knew it wasn't okay to beat up someone already not feeling well, but I also did not know how to help these people as a child. Thus, my curiosity about the human mind began: the development, psychopathology, and socioeconomic and cognitive factors. With every incident I heard or witnessed, I wondered how I could make a change. Thus, my pursuit of a career in mental health. As A psychiatry resident, I now have the knowledge and skill set to continue to make the changes I longed desire. I have been on multiple medical trips, and this time I will partner with the Ghana Mental Health Authority. This project will organize a trip to Ghana, West Africa, focusing on psychiatry to address the population's significant mental health challenges. In many regions of Ghana, mental health issues are stigmatized and underfunded, resulting in inadequate access to care and support. By providing psychiatric services, collaborating with local healthcare providers, and increasing awareness about mental health issues, this initiative aims to bridge the disparity. I kindly request a travel grant to support my initiative.
Medical students, mental health and primary care professionals, local communities in Ghana that are significantly impacted by mental illness are the beneficiaries of this initiative. Beginning in the capital of the nation, the initiative will expand to other municipalities. Participating resident physicians from the United States will also gain the knowledge and skills necessary to serve a healthcare system with limited resources and inadequate funding. The exposure of residents to a variety of clinical scenarios will enhance their diagnostic and therapeutic abilities. Interactions with local communities and professionals will foster cultural awareness, sensitivity, and competence. The initiative will establish and promote international connections between Ghanaian professionals, residents, and global mental health organizations. The objective of the initiative is to address critical mental health needs, enhance access to care, and increase understanding and awareness of mental health issues. By collaborating with local healthcare providers and psychiatric professionals, we aim to establish a lasting positive influence on mental healthcare in Ghana.
The initiative will directly benefit the local population by facilitating access to psychiatric care, frequently unavailable in these areas. This will enhance mental health outcomes and a higher quality of life for those with mental health disorders. By training and collaborating with local healthcare professionals, we enable them to sustainably improve mental healthcare delivery in Ghana and offer ongoing mental health services. Through our community outreach initiatives, we aim to diminish the stigma associated with mental health. This will spur more people to seek assistance when they require it, resulting in more prompt intervention and enhanced long-term results.
The knowledge and experience acquired through this endeavor will be disseminated to the mental community worldwide; expanding the scope and impact of mental health services worldwide can serve as a model for similar initiatives in other underserved regions.
By emphasizing community engagement and capacity development, we intend to leave an indelible mark on the mental health landscape of Ghana. This will be an ongoing initiative and partnership, and all parties will continue to reap the benefits of the knowledge and skills that this endeavor will produce.








A Glimpse into the Mental Health Landscape of Ghana
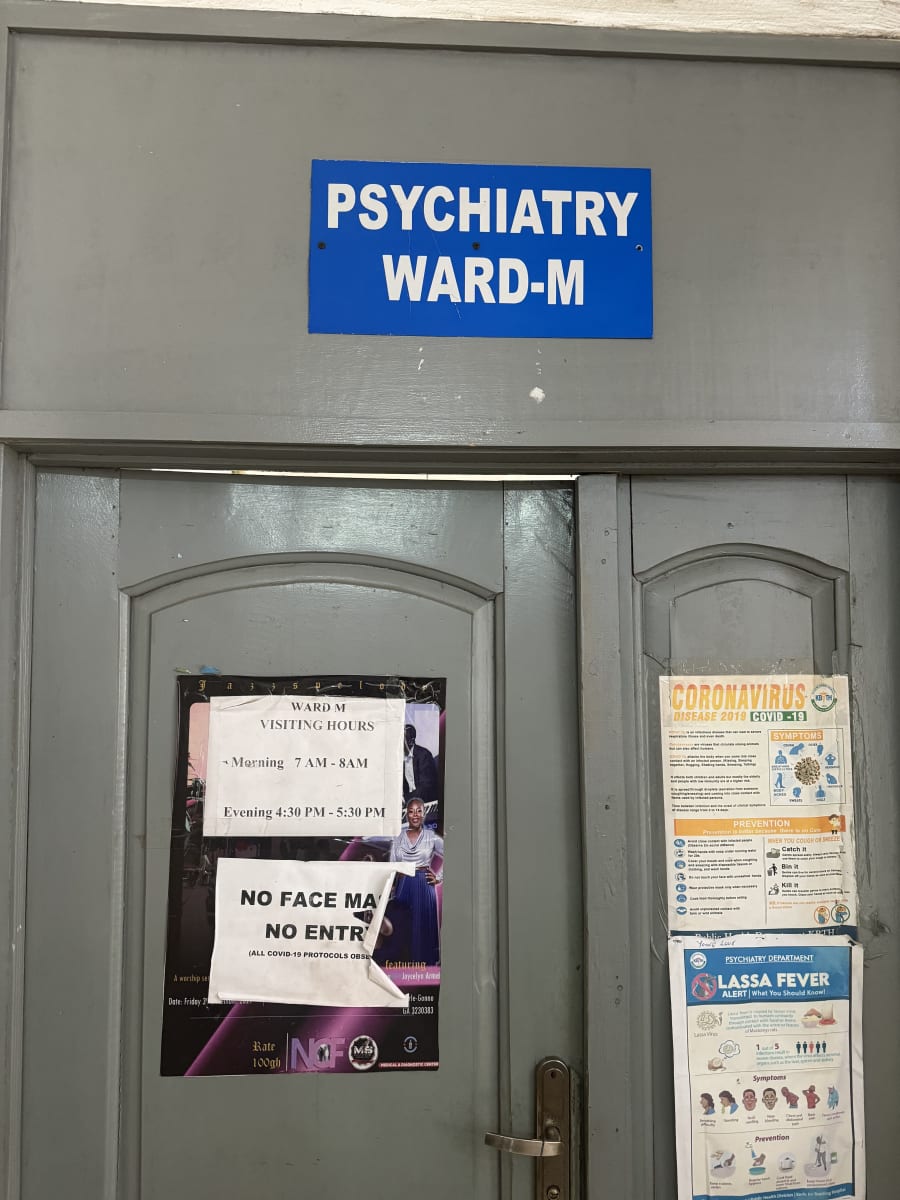
My journey through the varied domains of mental health in Ghana has been a profoundly enlightening experience, significantly expanding my understanding of mental health care on a global scale. During my clinical rotation across multiple hospital settings (forensic, outpatient, emergency, and inpatient), I have been privy to the extraordinary care mental health professionals deliver despite resource limitations. Their tenacity and commitment have been truly remarkable.
The first day of my rotation was marked by an interactive encounter with emergency services at the Accra Psychiatric Center. Within the dynamic setting of emergency psychiatry, practitioners exhibited remarkable proficiency in crisis intervention, stabilization, and appropriate medical service referrals. This was a case of a patient with a history of chronic alcohol use disorder who presented with symptoms of withdrawal, delirium and suspected hypovolemic shock. The patient was transferred promptly to the nearest regional hospital after being stabilized. As I transitioned to outpatient services, I observed mental health professionals' dedication to providing care in the community.
Notwithstanding their constrained resources, along with the health care providers, we implemented inventive approaches to engage and assist individuals requiring mental health services, emphasizing the importance of comprehensive and easily accessible services and, for instance, choosing a medication that is effective but also affordable and accessible to patient in their respective municipalities. Inpatient experiences, such as ward and teaching rounds, illuminate the difficulties of providing long-term patient care due to limited resources. The dedication to cultivating therapeutic milieus and nurturing a sense of community among individuals seeking mental health services exemplified the fundamental human-centered approach. During these rounds, I had the opportunity to share my knowledge and experience with house and medical officers and conduct complete psychiatric assessments.
Additionally, I had the privilege of contributing to forensic psychiatry cases in which experts navigated the complex interplay between mental health concerns and legal proceedings. This experience underscored the significance of interdisciplinary cooperation in the criminal justice system when addressing the complex requirements of individuals. It also highlighted the need for more psychiatrists in the country, as the psychiatric team was required to travel a three-hour distance to a different region of the country to provide the court with an expert report after evaluating and treating the patient who has driven a total of 5-6 hours to the psychiatric hospital for care regularly. I found it particularly remarkable how mental health professionals in Ghana provide high-quality treatment despite resource constraints. They prioritize preventive measures, emphasize community support, and ingeniously employ available resources to overcome the unique obstacles they face. Their capacity to achieve substantial results through resourcefulness and perseverance is genuinely praiseworthy.
Ghana, similar to numerous other nations, contends with fallacies about mental health. The persistence of stigma and stereotypes impedes the progress of opportune interventions and open dialogue. Engaging in conversations with professionals and community members has underscored the criticality of mental health education in debunking misconceptions and cultivating a nurturing atmosphere. During my time in Ghana, I became increasingly involved in clinical interviews, where I provided assessments on diagnoses, offered insights regarding modifying medication regimens, and offered my professional opinions. I was able to observe the complex labor of mental health professionals directly, which exposed the stark truth of a system contending with constraints, specifically regarding the availability of medications and affordability.
Notwithstanding the perceptive observations and precise diagnoses rendered by committed medical professionals, a substantial obstacle materialized—the lack of access to critical medications. Many factors, including limited treatment options and patients' financial limitations, caused this obstacle. There were cases where hospitals were compelled to withhold essential medicines from inpatients due to financial constraints.
One salient observation I made throughout my sojourn in Ghana was the notable preponderance of mental health specialists in Greater Accra and Ashanti. A population exceeding 34 million is attended to by an estimated 50 psychiatrists, resulting in the concentration of the preponderance of specialized care in these two regions. As a consequence, the remaining ten or more areas are severely deprived of essential psychiatric services.Moreover, it was apparent that there needed to be more specialized treatment in crucial fields, including addiction medicine, child and adolescent psychiatry, geriatrics, and consultation-liaison psychiatry (CL). The lack of specialized treatment in these domains presents a substantial obstacle in effectively attending to the varied and intricate mental health requirements of the populace. While acknowledging the exceptional commitment of mental health personnel in Ghana, it is imperative to recognize the systemic obstacles confronting this field. It is impossible to exaggerate the critical nature of enhancing medication accessibility and achieving a more equitable distribution of mental health professionals across regions. Furthermore, improving subspecialty care in pivotal domains will bolster the mental health system's overall comprehensiveness and adaptability. By disseminating these perspectives, I intend to illuminate the intricacies and potential for development within Ghana's mental health domain. Through the collective resolution of these obstacles, we can strive towards constructing a mental health infrastructure that is both fair and efficient, catering to the varied requirements of the entire populace.
An insightful exploration of the mental health sector in Ghana has unveiled the grit, empathy, and ingenuity exhibited by mental health practitioners amidst obstacles. Upon introspection of these encounters, it becomes apparent that the construction of a resilient mental health system that caters to the varied requirements of the populace necessitates proactive collaboration, ongoing education, and an empathetic demeanor. Ghana's narrative serves as a testament to the indomitable nature of the human spirit and the profound impact that specialized mental health care can have despite financial, cultural, and linguistic obstacles.