I am qualitatively exploring whether there are different patterns of access to care for undocumented individuals in Belize (individuals without Belizean social security identification) compared to Belizean nationals. We aim to identify differences in utilization of health services, differences in health care experiences, and other barriers to health access and care seeking. Additionally, we hope to identify any discrepancies between perceptions and experiences of healthcare access among undocumented populations in Belize versus what is offered. This will be accomplished by conducting semi-structured qualitative interviews with nationals and non-nationals residing in the Southern region of Belize. Interview questions will cover participants’ knowledge of what health services are available to them, as well as patient-provider, patient-facility, and patient-society barriers. Qualitative analysis will identify pertinent trends and/or disparities in health access between undocumented Belizeans and nationals.
Belize is primarily a country of destination for migrants transiting through Central America. Although efforts to expand asylum case processing capacity and grant a third national amnesty for asylum seekers in Belize have improved in recent years, the impact of legal status on health access in Belize is under-researched. Individuals residing in Belize who do not possess proper legal status are likely socioeconomically disadvantaged, or of racial and/or ethnic minorities. These populations often do not occupy positions of power or influence within Belize and their struggles often go unseen. By exploring and identifying access barriers, I hope to create a dialogue for lessening health disparities in Belize.
Pilot studies exploring the experiences of undocumented individuals accessing healthcare in multiple regions have identified preliminary evidence for the presence of significant health access barriers. Prior qualitative studies on health access in Belize have also alluded to a tiered health system with gaps in coverage even for nationals, more difficult access in areas without public clinics, and healthcare accessibility stratified by differences in socioeconomic status. Given this context, understanding how undocumented Belizeans access health services is essential not only to improve their health outcomes but also to assess systems-level drivers of healthcare utilization and associated costs. Existing literature in multiple regions already shows that investments in preventative care decrease health costs in the long term. Furthermore, upstream investments in bolstering civil registration and vitals statistics systems provide essential information for implementing focused public health policies that are ultimately more cost-effective long term. Findings from this study may directly influence public policies that improve health access for undocumented individuals in Belize.



















Belize is primarily a country of destination for migrants in Central America, historically attracting labor migrants of Mestizo, Mayan, or Garifuna descent from Guatemala, Honduras, and El Salvador seeking better economic opportunity. There were an estimated 40,000 to 60,000 irregular migrants residing in Belize in 2021. The 2022 Amnesty Program aimed to regularize at least 40,000 persons, however only received approximately 13,500 applications by the time the application period closed. Regularization via the Amnesty program is a multi-step process, and eventually allows for the individual to obtain a social security card, which is essential for work opportunities, education, and unencumbered healthcare access. Those who did not qualify for Amnesty included stateless persons who did not possess any forms of documentation or had difficulties obtaining documentation from their origin country, insufficient finances, fear of immigration authorities, and lack of awareness of the program. In October 2023, the Belizean government made public healthcare free to all, regardless of documentation status.
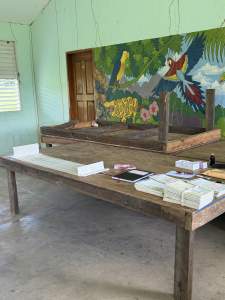
I conducted a qualitative study on healthcare access disparities for undocumented people residing in a historically under-resourced, rural region of Belize in collaboration with the Ministry of Health. Documentation status was defined in my study as having a valid social security card, as this card is necessary for accessing the full spectrum of public healthcare services available in Belize. During my time in country, I conducted 62 semi structured interviews across fifteen rural villages and three urban cities in the Toledo and Stann Creek districts of Belize. Interviews were conducted with undocumented persons, documented Belizeans, community health workers, health educators, physicians, nurses, hospital administrators, and Ministry of Health officials. Identification of villages with undocumented persons occurred with the assistance of regional health educators, who oversee the community health worker program. Identification and selection of undocumented and documented individuals were facilitated by community health workers and Humana People to People, a local NGO. These interviews were conducted via home visits, mobile vaccination clinics, charity clinics, and community centers within these villages. Undocumented individuals were primarily Kekchi Maya, Mopan Maya, Garifuna, and Mestizo migrants from Guatemala, Honduras, and El Salvador. Preliminary conclusions suggest that irrespective of documentation status, there exists common barriers to accessing healthcare in rural areas such as transportation costs, poor road conditions, clinical staffing and medication shortages, and language barriers. However, these difficulties are further exacerbated by lack of documentation, with undocumented individuals additionally endorsing the fear of deportation and discriminatory treatment by registration staff at public healthcare facilities. Ultimately, community health workers played a vital role as a liaison between vulnerable communities and healthcare services.
Additionally, I spent one week teaching the WHO/ICRC Basic Emergency Care course in Dangriga to 15 Belizean healthcare workers. The course aims to provide physicians and nurses with the skills to stabilize critically ill patients in resource limited settings.