With Drs. Tina Robison and Lindsey Beffa, I will help train midwives in Kigali, Rwanda in the "see and treat" method of surveillance of cervical dysplasia. Due in part to the rate of coinfection of HIV and HPV and reduced access to medical care, cervical cancer is the most common gynecologic cancer in Sub-Saharan Africa. By training providers to catch these processes before they progress, we can prevent this life-altering and sometimes life-ending diagnosis that most commonly occurs in reproductive age women. Cervical cancer is one of the few cancers that can be caught through surveillance and have significant effect on prognosis.
Additionally we hold lectures and journal clubs with the obstetrics and gynecology residency and the gynecologic oncology fellowship at the teaching hospitals in the city. This in person touch point dovetails with our Zoom monthly tumor boards through IGCS that are held.
Reproductive age women with and without HIV diagnosis. This is the patient population most affected with cervical dysplasia. These patients are often the primary caregivers and breadwinners in their family, and if they are diagnosed with cervical cancer and either (1) become disabled or infertile or (2) pass away from their diagnosis that family and community will be affected drastically.
This project is an ongoing partnership between gynecologic oncologists in the US and the women's providers of Rwanda. This partnership has been in place for over 7 years. The providers there on the ground have our contact information and touch base with us regularly. We additionally hold Tumor board conferences with the fellowship in Kigali to augment their training.

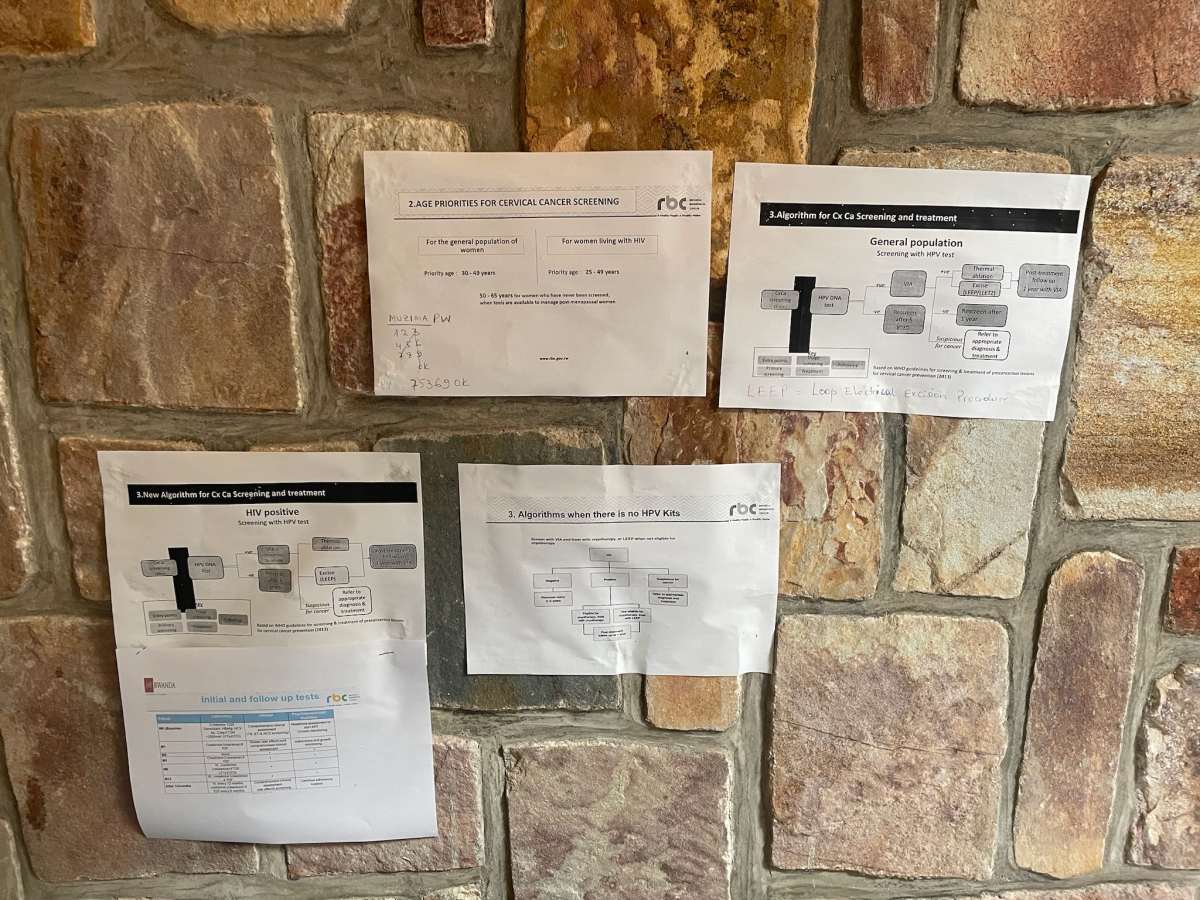




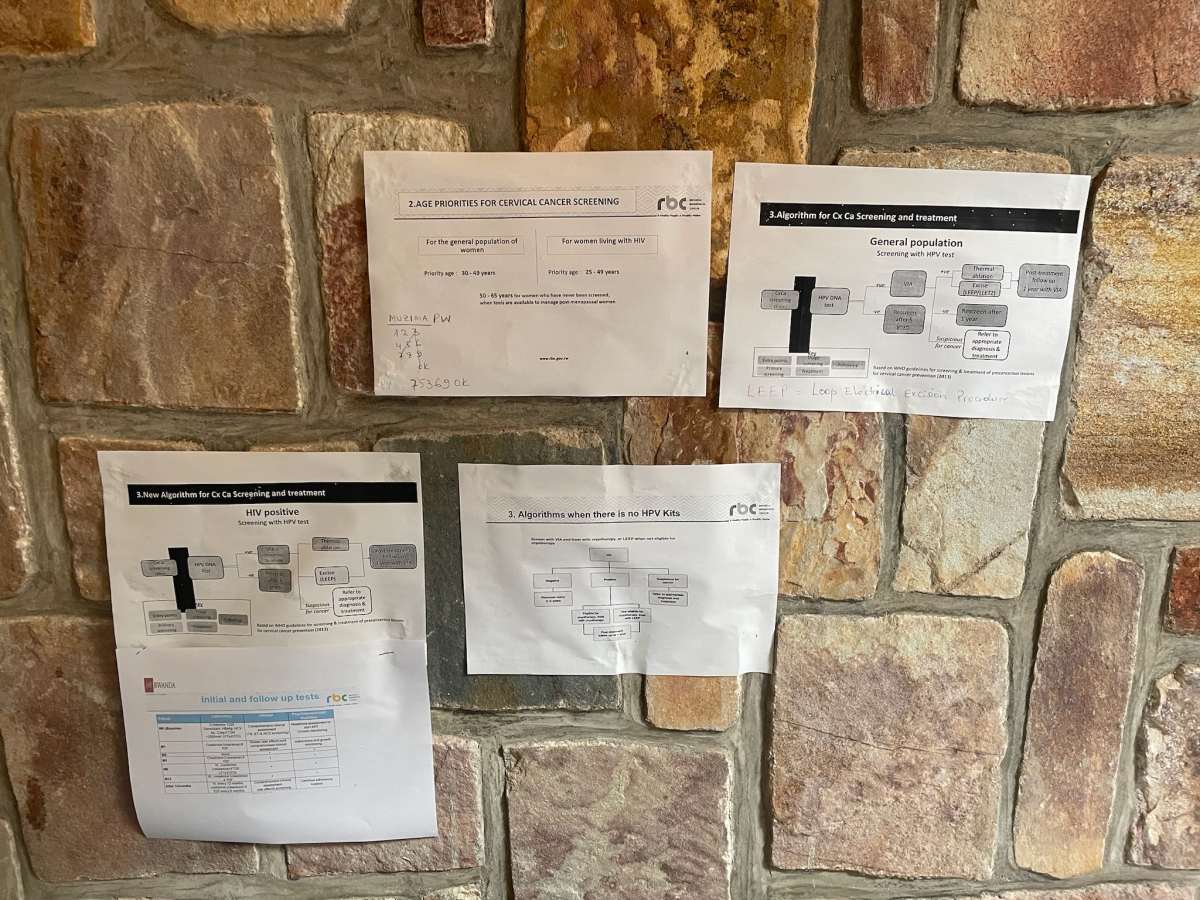





















We worked with local nurse midwives to train in cervical cancer screening. In a country with very few pathologists, Pap smears are difficult to access, so other screening modalities like “see and treat” and HPV tests are used. Patients with co infections of HIV and HPV carry a manyfold increased risk of cervical cancer, which is often a life altering or life ending diagnosis. We also worked with in country gyn oncologists, meeting for journal clubs, working in clinic and in the OR. Their program had graduated their first class of fellows, the first generation of in country trained gynecologic oncologists. Hopefully the first of many in a country that desperately needs providers.