There is currently an extreme shortage of anesthesia providers in eastern sub-Saharan Africa, with an average of 0.44 anesthesiologists per 100,000 people in Kenya compared to the 20.82 per 100,000 in the US. This is further skewed, with rural settings having even less surgical and anesthetic access [1].
However, even when anesthetic care is available, the risks involved are much greater in low-middle income countries compared to higher income countries. Maternal deaths due to epidural anesthesia occur 300 times more in low-middle income countries compared to the US , and deaths due to general anesthesia are 900 times more common [2].
As a result, we must focus on bringing safe anesthetic care to populations with low access to anesthetic care.. Part of the solution is to train qualified health care professionals how to safely administer anesthesia and empower them to work in multidisciplinary health care teams. The Kenya registered nurse anesthetist training program at Africa Inland Church (AIC) Kijabe Hospital located in Kijabe, Kenya is an 18 month training program that places trained anesthesia providers in rural hospitals after graduation.
In this project, I plan to work with the KRNA training program in the Kijabe Hospital by bringing my anesthesia training experience as a current US anesthesia resident. I plan to provide out of OR lectures on common anesthesia topics, as well as provide support intra-operatively. Doing so, I hope to supplement the education of the students in the KRNA program and further empower a system designed to address the scarcity and inadequacy of anesthesia services in highly needed areas.
[1] https://resources.wfsahq.org/anesthesia-and-analgesia/safe-anesthesia-care-in-western-kenya-a-preliminary-assessment-of-the-impact-of-nurse-anesthetists-at-multiple-levels-of-government-hospitals/
[2] https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(16)30003-1/fulltext
As stated above, there is a great need for safe anesthesia care in Eastern Africa. Training nurses to provide anesthesia care in these areas have been found to increase surgical volumes with fewer referrals to larger hospitals required due to the anesthesia gaps that had been addressed [1]. KRNAs trained by the Kijabe Hospital in particular are then placed in areas of greatest anesthesia need, who are to date providing care in 37 counties of Kenya, Somaliland, and South Sudan.
By working and training with the KRNAs, this project will directly affect their education through out of OR lectures and direct in-room support. This will add to their curriculum to produce competent and confident anesthesia providers. Further, the KRNAs will go on to serve in communities who desperately need anesthesia care. These KRNAs can also go on to become primary educators themselves in new facilities to train even more providers. Thus the indirect impact of this project can be exponential and help bridge the current health care disparity.
After reflecting on the potential harms of short term missions, particularly ones that are staffed with undertrained personnel offering services that either harm local communities or create a void once the mission teams leave, I became interested in creating long term, sustainable solutions to health challenges in lower resource settings. This trip will focus on creating a sustainable partnership with the hospital in Kenya, as we focus on training and empowering the local Kenyan CRNAs. The expected impact will be to further a system built to empower a local community to remain self sufficient.
On a more personal level, I hope to strengthen my skills and training as an anesthesiologist by working in a different setting than I am used to, which will force me to think deeper and more critically about peri-operative issues, and be creative in my solutions. Second, I hope to gain a deeper cultural understanding of the people of Kijabe and learn how social and cultural factors affect health and the practice of health care in this community. Not only does this bring me great personal satisfaction, but it also helps prepare me for future international experiences.
Beyond residency, I hope to be involved in similar sustainable efforts, such as training international providers and spending a few months of the year on site. As the need for global surgery increases, so does the need for safe anesthesia practices and capable anesthesiologists. I believe that the ability to access safe healthcare, including surgery, is a universal human right, and feel impassioned to lead a career with a global health focus.




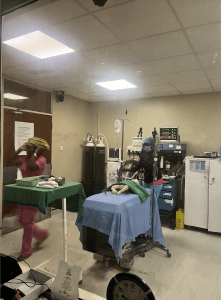



We worked closely with the anesthesia physician residents and the KRNA students, by offering in room super vision and discussion. We oversaw and taught regional blocks intra operatively and post operatively. We also participated in a simulation course for physicians and KRNAs in the Kenya area for pediatric simulation. We ran scenarios and debriefed afterwards.