I will be teaching Pediatric Advanced Life Support (PALS) to pediatric physicians at the Mongolian National University of Medical Sciences using an innovative, simulation-based curriculum. Although this is not an officially sponsored American Heart Association (AHA) course due to funding limitations, we will be using AHA PALS principles, algorithms, and teaching methods to deliver high-quality, evidence-based resuscitation education. This course is especially significant as there are currently no certified AHA PALS programs in Mongolia, making this a unique and much-needed educational opportunity for local learners.
The course will incorporate both high- and low-fidelity simulation trainers to enhance hands-on skills and reinforce critical thinking during pediatric resuscitations. Sessions will include structured debriefing to help learners reflect on their performance and solidify key take-home points. Topics will cover recognition of respiratory failure, shock, and cardiac arrest, as well as team dynamics and effective communication in emergency situations.
To ensure that learners have access to reliable reference materials, I have raised $1,000 in external funds to purchase AHA-certified PALS textbooks, posters, and additional learning aids. These resources will be distributed to participants and used to support both the didactic and simulation components of the course.
By teaching evidence-based resuscitation techniques in a structured, immersive environment, this course will help equip pediatric physicians with the skills and knowledge needed to respond confidently and effectively to critically ill children. Ultimately, this training will make a meaningful difference by improving outcomes and saving the lives of children who present with cardiopulmonary compromise.
This project will directly benefit pediatric physicians, pediatric residents, and emergency medicine providers at the Mongolian National University of Medical Sciences (MNUMS), as well as indirectly benefit the pediatric patients they care for across Mongolia. This is a critical population to target because Mongolia currently lacks access to formal Pediatric Advanced Life Support (PALS) training. There are no certified AHA PALS programs in the country, and many providers have not received structured training in evidence-based pediatric resuscitation techniques.
Pediatric providers in Mongolia face unique challenges, including limited resources, long distances between healthcare facilities, and high rates of pediatric morbidity and mortality in rural and underserved regions. Many pediatric emergencies—such as respiratory failure, shock, and cardiac arrest—require immediate and well-coordinated interventions to prevent poor outcomes. Without appropriate training in systematic assessment and team-based response, providers may lack the skills and confidence to respond effectively to life-threatening situations.
By providing simulation-based PALS education tailored to local needs, this program will strengthen the ability of Mongolian pediatric providers to recognize and manage critically ill children. The course will also promote a culture of teamwork, communication, and preparedness, which are essential for improving outcomes in high-stress situations.
The expected impact of this project is both immediate and sustainable. In the short term, pediatric physicians and trainees at the Mongolian National University of Medical Sciences will gain essential skills in recognizing and managing pediatric cardiopulmonary emergencies using evidence-based Pediatric Advanced Life Support (PALS) principles. Through simulation-based training, learners will improve their clinical decision-making, teamwork, and confidence in high-stakes situations. This will directly enhance the quality of pediatric emergency care and has the potential to reduce preventable deaths among children presenting with respiratory failure, shock, or cardiac arrest.
Longer term, the goal is to foster a core group of local champions in pediatric resuscitation who can carry the work forward after my departure. I will be providing teaching guides, debriefing tools, and structured curricula that they can continue to use and adapt locally. Additionally, the AHA-certified textbooks, posters, and learning materials purchased with externally raised funds will remain on-site as a permanent resource for ongoing practice, review, and peer education.
This foundational course may serve as a springboard for developing a sustainable, locally-led pediatric resuscitation education program in Mongolia. By investing in the professional development of local providers and leaving behind the tools and knowledge needed to continue the training, the project aims to build long-term capacity. The learners will not only use their skills in clinical care but also help train future generations of pediatricians, creating a ripple effect that can improve child health outcomes across the region.











Individuals and Communities Impacted
This global health educational mission to Ulaanbaatar, Mongolia, supported by the Dox Foundation, had a profound and multifaceted impact on both learners and the broader academic and healthcare communities within the Department of Pediatrics at the Mongolian National University of Medical Sciences (MNUMS).
Our participants represented a diverse cross-section of pediatric care in Mongolia, including faculty physicians and trainees in general pediatrics and pediatric critical care medicine. These individuals are responsible for the care of some of the most vulnerable children in Mongolia, and they serve as the next generation of clinical educators and leaders who will continue to expand pediatric education and improve patient outcomes across the country. Some traveled many hours to attend.
Over the course of four intensive educational days, our multidisciplinary U.S.–Mongolian team engaged learners through structured workshops, lectures, and simulation-based sessions designed to improve clinical and teaching competencies.
1. Pediatric Resuscitation and Critical Care Providers
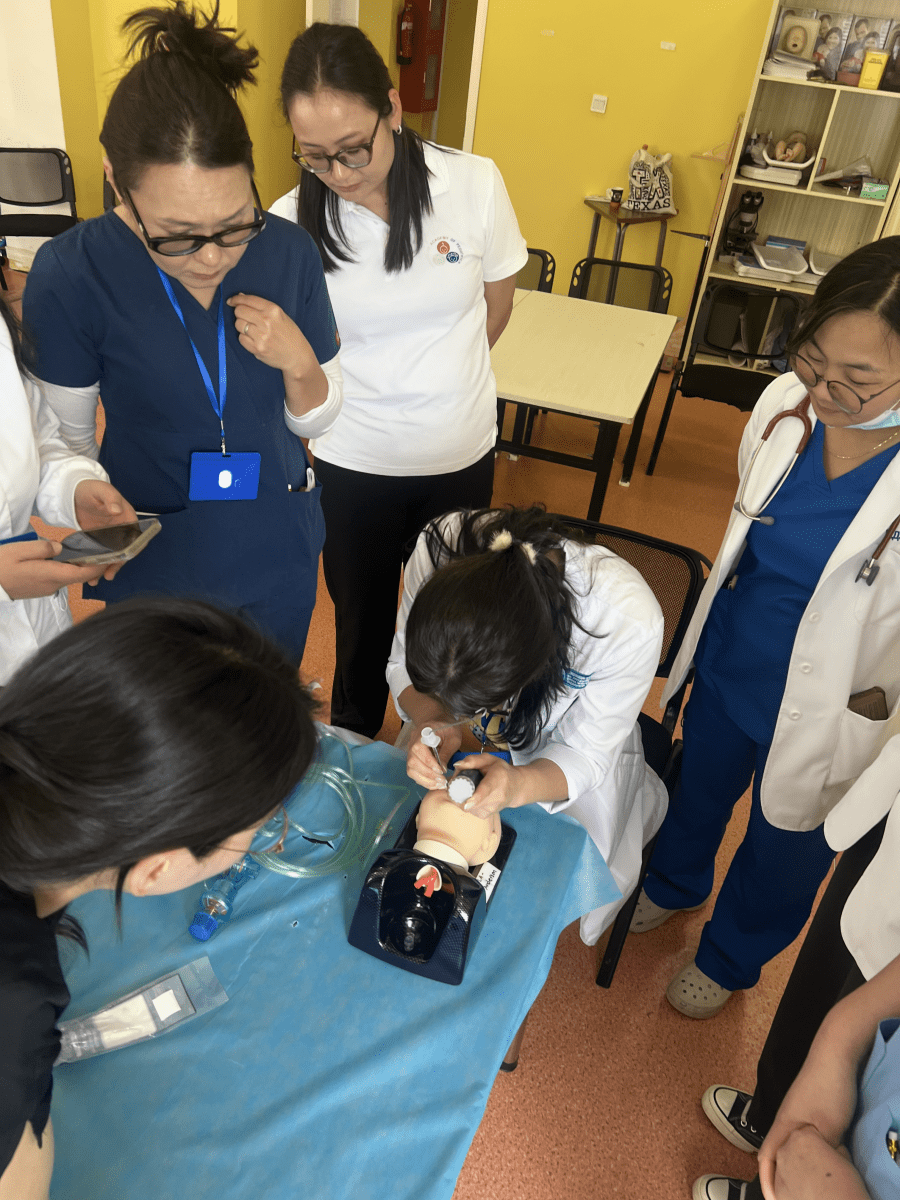
The first two days focused on pediatric resuscitation training, a key area of need identified by the host institution. Using a hybrid didactic and simulation format, participants learned and practiced high-priority pediatric resuscitation techniques using low-fidelity simulation models, checklists, and established clinical algorithms. The training emphasized not only technical skill acquisition but also crisis resource management—team communication, role clarity, and leadership during high-stakes resuscitations.
Participants found the practical, hands-on approach especially valuable. The sessions provided a framework for managing acutely ill children and strengthened their confidence in recognizing and responding to pediatric emergencies.
Immediate feedback collected through QR-code evaluations revealed overwhelming satisfaction and appreciation for the training. Learners reported that the opportunity to repeatedly practice scenarios in a supportive, nonjudgmental environment helped consolidate knowledge and improve teamwork skills. Several faculty participants have since expressed interest in integrating these approaches into their own teaching.
2. Simulation Educators and Academic Faculty
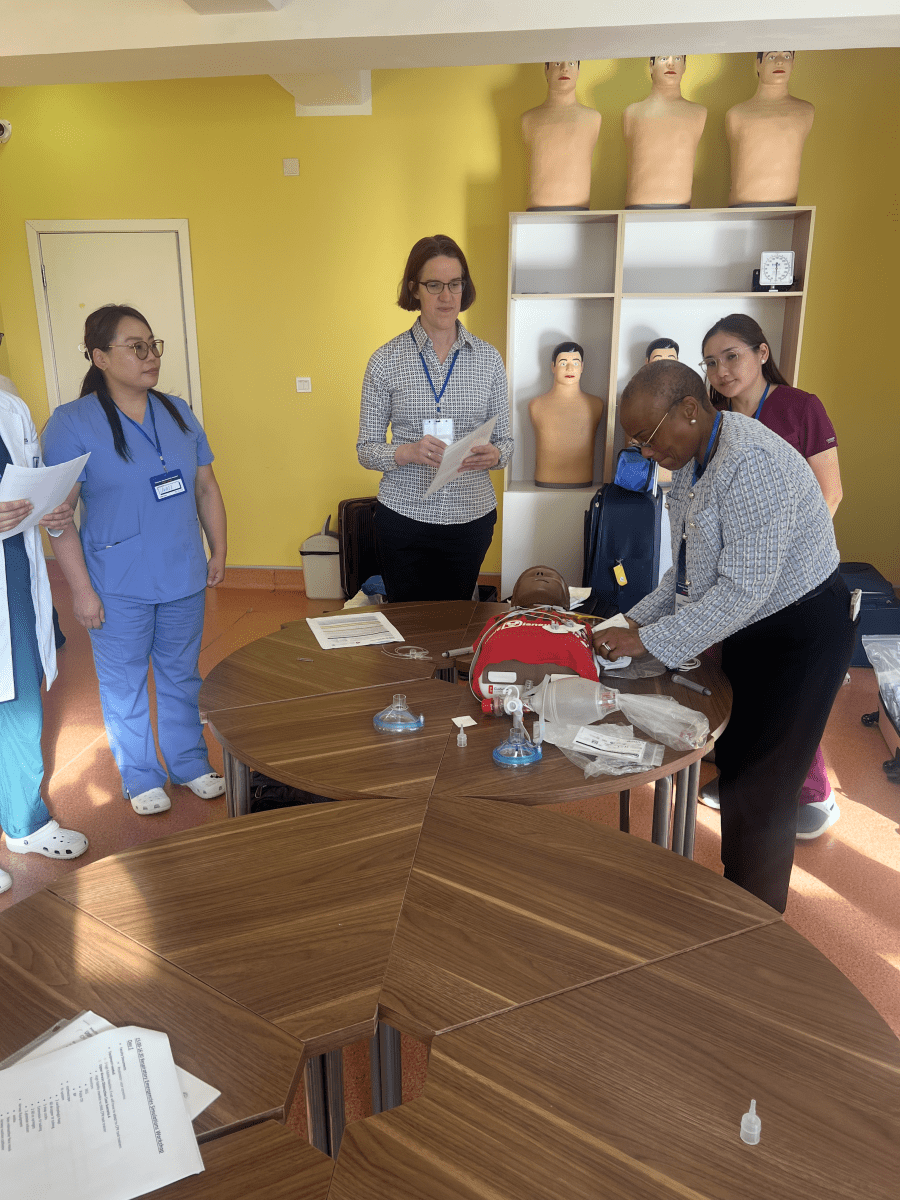
On the third day, the focus shifted toward simulation-based education—an area that remains in early development in the department of pediatrics. Learners participated in an all-day Simulation Educator Course that introduced the fundamentals of simulation pedagogy, including scenario design, debriefing techniques, and methods for evaluating learner performance.
Through interactive workshops and small-group discussions, participants gained hands-on experience in conducting debriefings, analyzing performance gaps, and fostering reflective learning. The session also explored the use of artificial intelligence (AI) tools to simulate patient encounters, demonstrating how these technologies can augment history-taking and physical examination training for medical students.
For many faculty members, this was their first exposure to structured simulation-based education. The enthusiasm and engagement were striking—participants eagerly discussed how they could adapt these strategies to the local context. By the end of the session, several faculty groups had begun planning how to incorporate simulation and debriefing principles into their teaching curriculum.
3. General Pediatric Faculty and Trainees
The mission concluded with an all-day pediatric didactic session, featuring a series of lectures on high-yield general pediatrics topics. This portion reached a broader audience within the Department of Pediatrics.
The interactive nature of these lectures—emphasizing case discussions, evidence-based approaches, and cross-cultural exchange—helped to reinforce the clinical material presented during the resuscitation and simulation sessions. Learners reported that the combination of lectures and simulation practice deepened their understanding and retention of key pediatric principles.
4. Institutional and System-Level Impact
Beyond the direct participants, this mission created a ripple effect within the MNUMS pediatric community. Faculty leaders expressed enthusiasm for expanding pediatric resuscitation and requested continued collaboration to build a sustainable simulation training infrastructure.
In response, our team developed a longitudinal learning plan through 2026, providing structured review materials, teaching guides, and stepwise goals for progressively advanced training modules. This sustainability plan ensures that the skills and knowledge gained during this mission will continue to grow and evolve even between in-person visits.
The collaboration also strengthened institutional ties between MNUMS and U.S. academic centers, fostering opportunities for ongoing mentorship, joint research, and shared educational initiatives. Several participants have already reached out to explore future virtual workshops and faculty exchange programs.
5. Broader Educational and Emotional Impact
Equally important was the intangible impact of shared purpose, cultural exchange, and professional connection. The Mongolian learners demonstrated remarkable dedication and curiosity, often staying long hours to continue discussions and practice scenarios. Many described the experience as enhancing their clinical confidence.
For the visiting faculty, the experience reinforced the universal nature of medicine and the power of education to transcend language and geography. The collaboration cultivated mutual respect and understanding, highlighting how innovation and compassion can thrive even in resource-limited environments when knowledge is shared freely and authentically.
6. Summary of Impact
• Direct participants: Faculty and trainees from the Department of Pediatrics, MNUMS
• Disciplines represented: General Pediatrics and Pediatric Critical Care Medicine
• Educational reach: Over 50 participants engaged through didactic, simulation, and educator training sessions
• Educational structure: 2-day Pediatric Resuscitation Workshop, 1-day Simulation Educator Course, and 1-day Pediatric Lecture Series
• Outcomes: Improved confidence, technical skills, and understanding of resuscitation and simulation-based education
• Sustainability: Established a multi-year learning plan through 2026 to maintain and expand the educational foundation
• Long-term value: Strengthened institutional capacity, enhanced quality of pediatric care, and fostered international academic collaboration
Conclusion
The individuals most directly impacted by this mission were the faculty and trainees of the Department of Pediatrics at MNUMS, representing both general pediatrics and pediatric critical care medicine. Through immersive teaching, active simulation, and open dialogue, these participants gained not only new technical skills but also the tools and confidence to become educators themselves.
The ripple effect of this mission extends beyond individual learners—it strengthens the pediatric education infrastructure in Mongolia and lays the groundwork for sustainable, locally driven improvements in child health. By empowering providers through education, this collaboration aligns with a shared vision: to ensure that every child, regardless of geography, has access to safe, effective, and compassionate care.