This project aims to build capacity and expand our Global psychiatric and addiction education program across two countries, in multiple cities, including Cape Coast, Accra, and Abuja, by combining clinical training, faith-based engagement, and community health fairs. We will deliver diagnostics for trainees and clinicians, including screening and brief interventions, patient care, destigmatizing mental illness, and building referral pathways. We will identify local clinicians and faith champions, and continue to develop the mentorship network to sustain momentum and strengthen collaboration across Ghana and Nigeria.
We aim to train ~300 trainees including Level 400 and 500 medical students of UCC, clinicians, and faith leaders, and directly engage over 1,000 community members. The three training sites collectively serve a catchment population of >500,000 people, meaning our trained champions will impact a large, underserved population well beyond the initial visit.
We expect to see ≥30% improvement in knowledge, confidence, and stigma reduction scores among trainees based on pre-/post-surveys. Patient care activities will impact at least 1,000 individuals, connecting them with trained clinicians. A cross-country mentorship program will continue for six months to reinforce skills and encourage case-based learning. Outcomes will be shared with peers and colleagues in psychiatry at a conference. Each region will retain local clinicians and faith champions, along with training materials, to ensure the long-term benefits of the project are sustained. We will hold bimonthly mentorship calls for six months following the trip to support implementation, troubleshoot barriers, and share data. By integrating faith leaders into the care pathway and leaving behind reusable resources, the project builds a self-sustaining model that strengthens both community and clinical capacity.
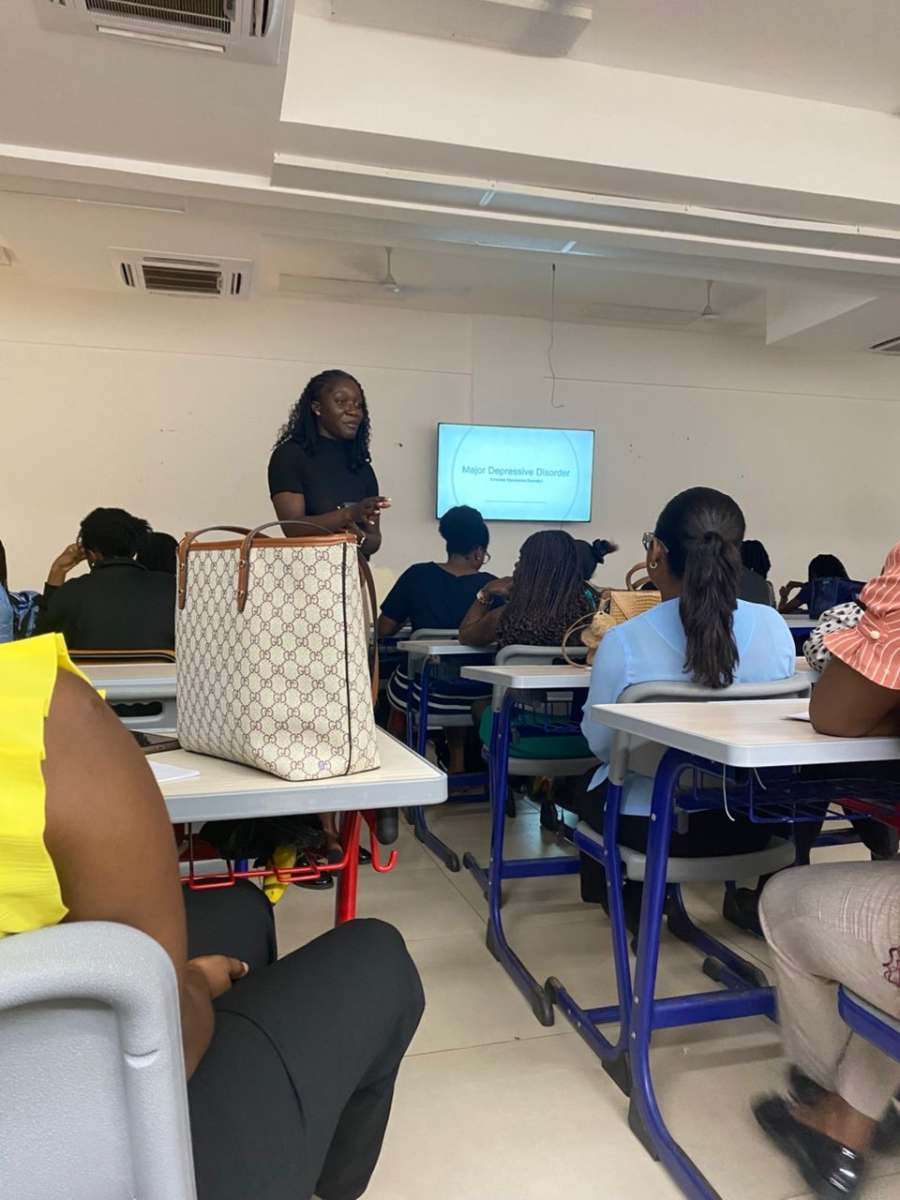





I engaged in clinical and educational work, contributing meaningfully in academic, clinical, research, community, and faith contexts. I provided structured teaching at two medical schools, delivering sessions on psychiatric disorders. I collaborated on complex diagnostic cases and treatment planning for patients while teaching on clinical rounds in multiple psychiatric hospitals. In collaboration with student and resident organizations, we initiated research and exchange trainee efforts focused on mental health and addiction literacy, treatment barriers, and the integration of psychiatric care into primary and faith-based settings. Engagement in faith settings, a trusted space in the communities I served, helps advance culturally grounded discussions on mental health, addiction, stigma, and pathways to care. Throughout these experiences, I am reminded of what it means to exemplify strong clinical judgment, cultural humility, and a clear commitment to developing sustainable and equitable mental health and addiction services in underserved communities.