For my global health elective, I will travel to The Gambia as a PGY-2 Emergency Medicine resident to support a collaborative training initiative between UC-Davis, UH-Cleveland, and local clinicians. My goal is to bring the skills I am developing in emergency medicine—particularly point-of-care ultrasound (POCUS)—to a setting where formal EM training does not yet exist and resources are limited.
During my time at Edward Francis Small Teaching Hospital and affiliated sites, I will help lead hands-on POCUS sessions focused on core applications such as basic echocardiography, IVC assessment, trauma evaluation, and procedural guidance. POCUS is uniquely powerful in low-resource settings: it allows rapid bedside assessment of critically ill patients, improves diagnostic accuracy, and can be used virtually anywhere—even outside the hospital—when radiology services or advanced imaging are unavailable. By training Gambian physicians, nurses, and clinical officers to confidently incorporate POCUS into their daily practice, we can enhance emergency care capacity long after our team leaves.
This project will make a difference by strengthening the local healthcare workforce rather than providing short-term care. Improving diagnostic capabilities directly impacts patient outcomes in time-sensitive conditions such as shock, trauma, and obstetric emergencies. The goal is to empower clinicians with sustainable, practical tools that fit their environment and expand their ability to deliver high-quality emergency care. With support from this scholarship, I hope to contribute meaningfully to a growing foundation of emergency medicine in The Gambia and help build long-term, locally driven improvements in patient care.
The people of The Gambia will benefit from improved access to timely and accurate emergency care in a country facing significant resource limitations. With a population of 2.8 million, nearly 30% living below the international poverty line, and only 1.52% of the national GDP spent on health—far below the WHO’s recommended 5%—patients often present late in illness and with minimal diagnostic support. Although life expectancy has risen from 31.2 years in 1950 to 65.9 years in 2023, the healthcare system continues to face gaps in emergency care and rising new health threats. Expanding point-of-care ultrasound (POCUS) helps fill these gaps by improving diagnostic accuracy, reducing unnecessary procedures, and guiding faster, safer treatment decisions in settings where advanced imaging is unavailable.
Gambian healthcare professionals—physicians, nurses, and clinical officers—are equally central to this effort. With no formal emergency medicine training pathway and limited imaging resources, clinicians are often forced to rely on clinical judgment alone for time-sensitive decisions. Training providers to use POCUS builds confidence, enhances their ability to diagnose emergent conditions, and equips them with a sustainable skill that can be used anywhere a patient is located. The goal is to create a self-sustaining educational framework in which local clinicians can continue teaching future generations, strengthening emergency care capacity from within.
These populations were chosen because improving diagnostic capability benefits patients immediately while empowering clinicians ensures long-term, systemwide improvement. Strengthening both sides—care recipients and care providers—creates the most durable impact on health outcomes in The Gambia.
The expected impact of this project is a lasting improvement in The Gambia’s emergency care capacity through sustainable POCUS training. Rather than providing short-term clinical care, this elective focuses on education, skill-building, and empowering Gambian healthcare professionals to independently diagnose and manage emergent conditions using ultrasound. By strengthening diagnostic accuracy in low-resource settings, the project directly improves patient outcomes, reduces unnecessary procedures, and supports faster, safer decision-making across emergency and acute care environments.
A key goal is to help build a training program that becomes fully self-sustaining. By teaching foundational POCUS skills to current clinicians and identifying local champions who can continue the instruction, this initiative aims to create a system in which Gambian providers become the long-term trainers for their colleagues and future generations. This approach promotes confidence, competence, and resilience within the healthcare workforce and helps ensure that POCUS becomes a routine, reliable tool in emergency and primary care throughout the country.
The learnings from this experience will carry forward after I return by strengthening my ability to teach POCUS, adapt EM practices to low-resource settings, and collaborate effectively in global health partnerships. I plan to continue supporting the program remotely, contribute to curriculum development, assist future trainees who travel to The Gambia, and help build continuity between visiting teams. The goal is for each rotation to advance the program a little further, ultimately supporting Gambian clinicians in leading and expanding their own emergency ultrasound training efforts.













My two-week elective in The Gambia was an incredibly impactful and humbling experience centered on sustainable POCUS education and hands-on clinical application.
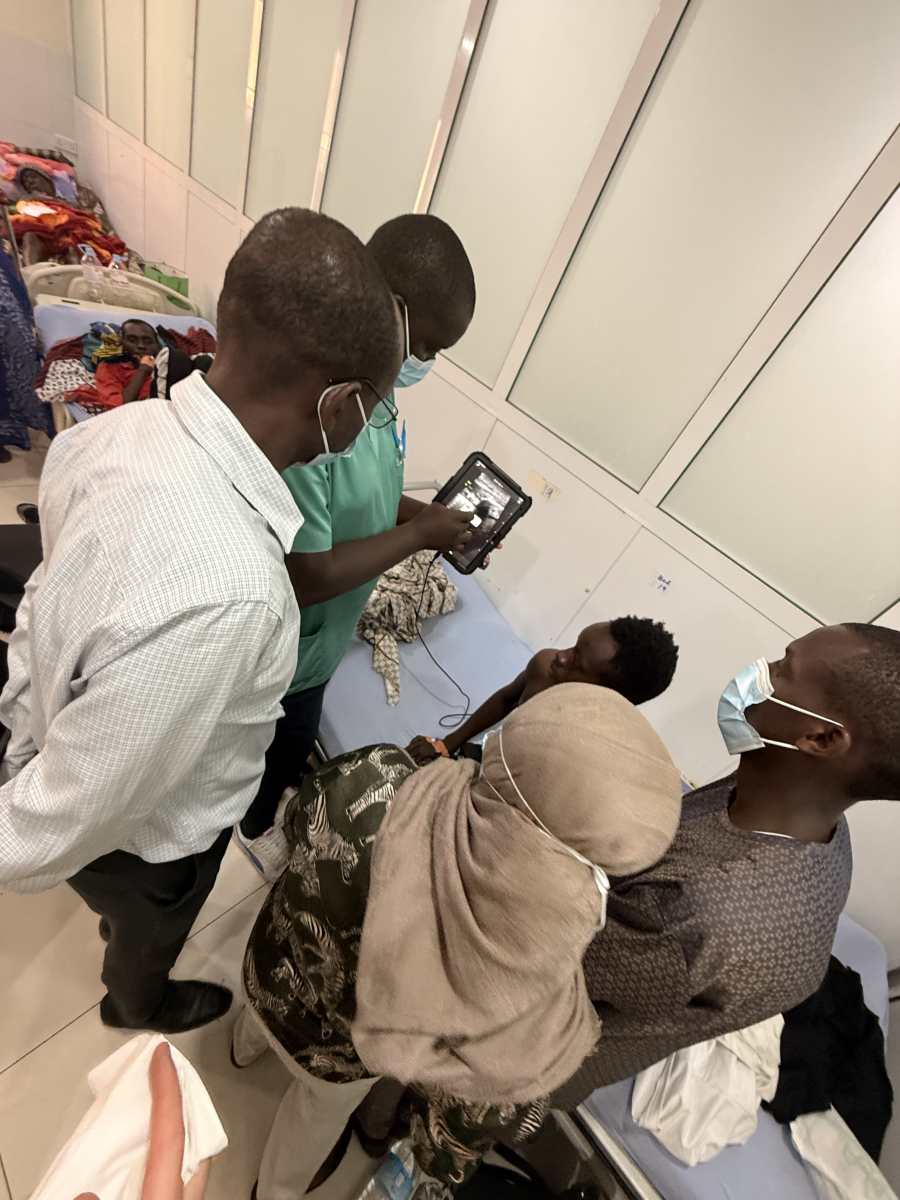
During the first week, we provided focused POCUS training to surgeons, anesthesiologists, and radiologists. Teaching sessions combined didactics with bedside application, allowing participants to immediately integrate skills into patient care. Core topics included the FAST exam, abdominal ultrasound for small bowel obstruction and intussusception, procedural guidance, and the CURLS protocol for rapid cardiac and IVC assessment. The training directly influenced clinical decision-making, equipping physicians with practical tools to improve diagnostic accuracy and guide timely interventions for their patients.
In the second week, we worked primarily with internal medicine physicians, pediatricians, and radiologists. Educational focus shifted to cardiac and IVC ultrasound, thoracic/lung ultrasound, and structured shock evaluation. Again, teaching was paired with real-time bedside scanning, reinforcing skill acquisition through direct patient care.
The impact was both immediate and tangible. We identified a large pericardial effusion in a postpartum mother, expediting appropriate management. In another case, ultrasound helped diagnose intussusception in a pediatric patient, allowing timely surgical intervention. These moments highlighted how powerful bedside ultrasound can be in resource-limited settings and how education translates directly into improved patient outcomes.
The physicians were deeply engaged, grateful, and eager to incorporate their new skills into daily practice. Watching their confidence grow over just two weeks was inspiring. It was an amazing privilege to contribute to capacity-building efforts that will continue benefiting both providers and the people of The Gambia long after our departure.