1. Identify and implement educational measures to enhance intensive care unit support for Malawian children at Kamuzu Central Hospital, Malawi.
2. Educate Malawian anesthesia clinical officers through lectures, hands-on training and a low-fidelity simulation curriculum.
3. Provide anesthesia, analgesia, and sedation for Malawian patients undergoing surgical procedures and those admitted to the intensive care unit of Kamuzu Central Hospital, Malawi.
Kamuzu Central Hospital (KCH) serves a population of about 5 million people, and is a referral center for the central region of Malawi. The intensive care unit (ICU) of the hospital admits approximately 50 pediatric patients annually, with significant seasonal variation related to malaria burden and traumatic injury.
The pediatric educational quality improvement initiatives of this project will directly benefit the children of Malawi admitted to this ICU. The clinical education component for Malawian anesthesia clinical officers will benefit all Malawians as these students are the future providers of anesthesia care throughout the country. The direct anesthesia care I will be providing during the trip will benefit all Malawians currently receiving care in this hospital, particularly obstetric and pediatric surgical patients.
The past five years has shown a dramatic decline in inpatient pediatric mortality at KCH, that reflect the nationwide improvements. The mortality rate has decreased from about 8% in 2012 to a recent rate of about 3.5% found on an audit of the charts of deceased patients over a 13-month period from November 2104 to December 2015. However, very little data exists on the mortality rate of children receiving care in the KCH ICU, and there is significant variability in the conditions necessitating ICU admission, extent and duration of care provided, and ICU providers’ pediatric knowledge base and skills in this mixed adult and pediatric unit.
In order to continue to decrease mortality rates, efforts need to be focused on identifying gaps in knowledge in providing care for children admitted to the ICU and subsequently improving outcomes. To do this, ICU providers’ self-reported areas of need will drive initial educational interventions.
Through this mission, we aim to impact care through the following objectives:
(1) Address current provider-identified gaps in knowledge regarding pediatric critical care for KHC ICU pediatric patients through educational quality improvement interventions.
(2) Identify deviations from recognized age and weight-based respiratory support, airway management, sedation, nutrition, and fluid administration via retrospective chart review of KCH ICU pediatric patients.
(3) Improve pediatric outcomes by developing and implementing educational interventions targeting age and weight-based respiratory support, airway management, sedation, nutrition, and fluid administration will result in increased provider confidence, and standardized care.
In addition to sustained improvement in pediatric ICU outcomes, we anticipate impacting medical education of native practitioners and students by providing evidence based, self-sustaining training.



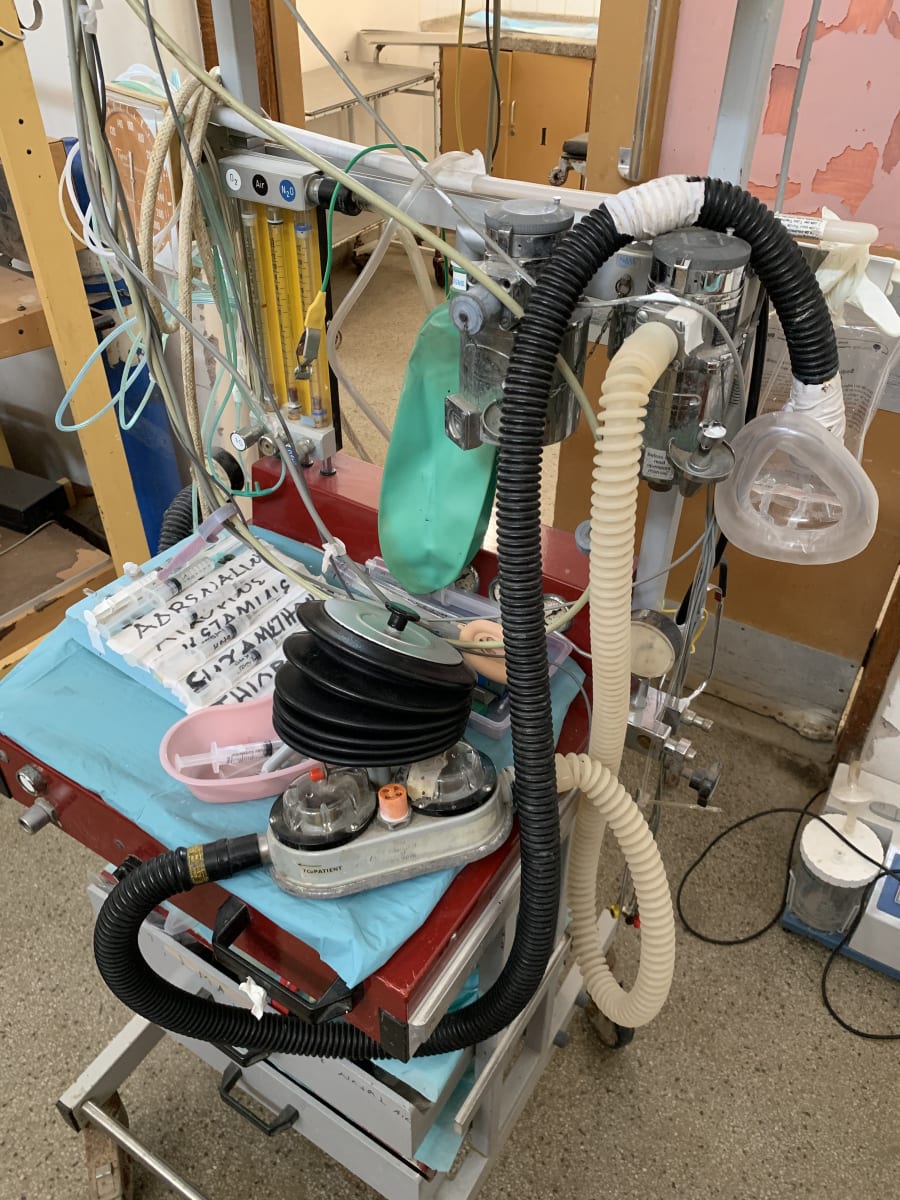




This was an incredible opportunity to launch a project with the potential for lasting improvement in provider education and pediatric ICU care. My time in the operating theater directly impacted all patients undergoing procedures requiring anesthesia and analgesia. However, I was personally impacted the most through the work we were able to do on this trip. The challenges of providing care in a critically limited resource environment have made me a morally and mentally stronger physician.