I will be working at the University Teaching Hospital of Kigali in Rwanda to teach principles and techniques of pediatric anesthesia to local anesthesia providers. My colleague, Dr. Amy Cassidy, is currently a Fulbright scholar in Kigali for a year with the goal of improving maternal and peripartum care. Dr. Cassidy’s specialty is obstetric anesthesiology and asked me, as a board-certified pediatric anesthesiologist with over seven years of experience, to assist her in improving neonatal and pediatric anesthesia care. I will teach pediatric principles, pediatric airway & anesthesia skills, and Pediatric Advanced Life support. This will occur onsite at the hospital in the perioperative area as well as in the operating rooms. Several physicians from different anesthesiology subspecialties will be visiting Dr. Cassidy throughout her year in Kigali; however, I will be the only certified pediatric anesthesiologist to work with her on site.
The University Teaching Hospital of Kigali (CHUK) is run by local healthcare professionals. The volunteers work alongside them to assist with education and training and to introduce up-to-date medical practices. Established in 1918, CHUK is the largest referral hospital in Rwanda with over 500 inpatient beds. The anesthesia providers are from Rwanda and will remain in Rwanda to continue their practice. Very few to no local anesthesiology providers have specialty training in pediatric anesthesiology and there is a great need for instruction in this area.
The goal of this trip is to increase knowledge of pediatric anesthesia principles and help establish protocols to improve patient care. The expected impact is to decrease mortality and morbidity in the pediatric and neonatal population that can continue to occur after I return home.























I was fortunate to travel to Kigali, Rwanda, in March 2020 to teach pediatric anesthesia skills to the anesthesiology faculty and staff at the University Central Hospital of Kigali (CHUK). My trip was planned around visiting a colleague who is a Fulbright scholar for obstetric anesthesiology for the year. With her coordination, several subspecialists in anesthesiology have visited during her year in Kigali to share their knowledge and expertise.
Originally built in 1918, the University Central Hospital of Kigali (CHUK) is the largest referral hospital in Rwanda with over 500 beds. Located in central Rwanda, its mission is to provide quality health care to all Rwandans irrespective of socioeconomic status through a commitment to training medical professionals according to international standards. The CHUK anesthesiology department encompasses a variety of health professionals to include medical students, nurse anesthetists, anesthesia residents and physician anesthesiologists. I had the privilege of working with the first certified anesthesiologist in Rwanda and the first and only pediatric trained anesthesiologist in the country.
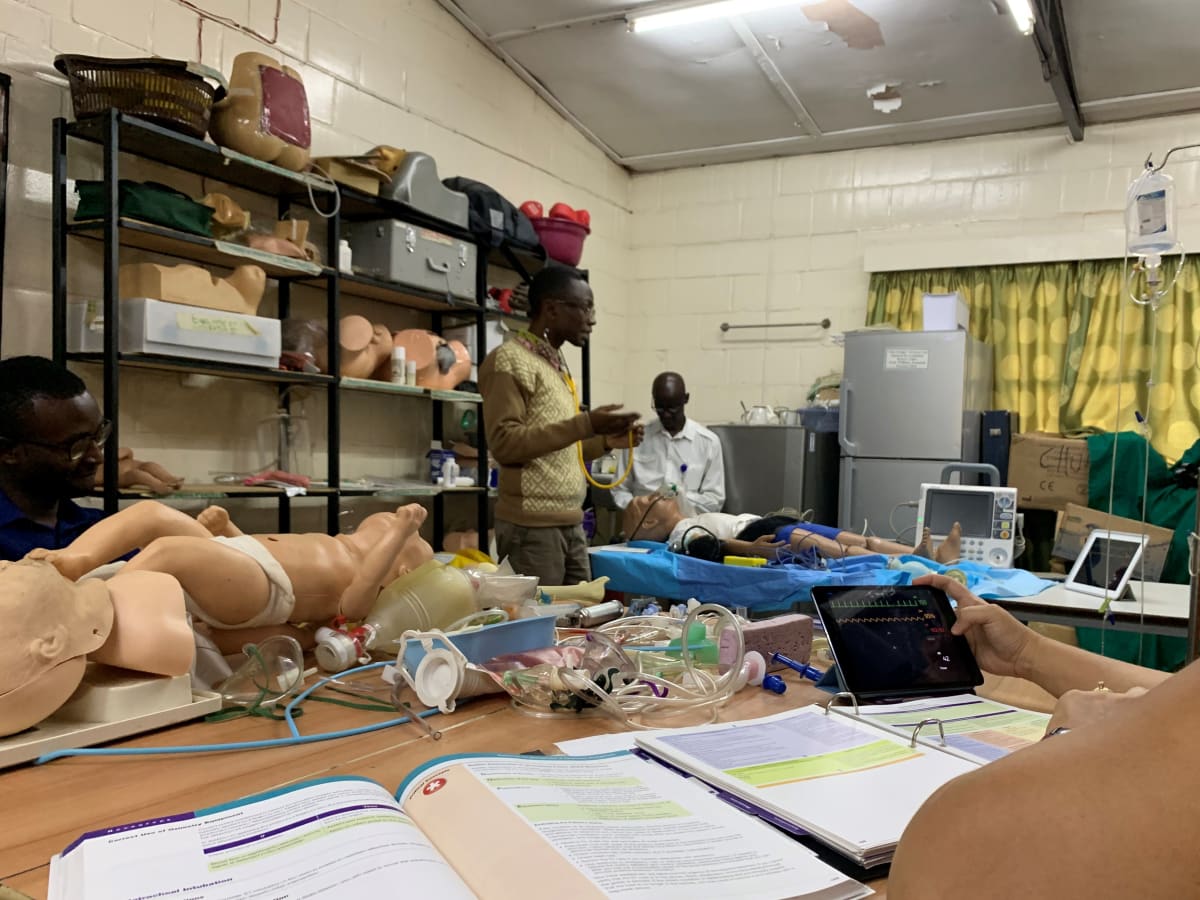
As a visiting pediatric anesthesiologist, I was asked and gave two grand rounds lectures to the anesthesiology department concerning pediatric airway management and providing pediatric anesthesia care in low resource settings. After presenting morning lecture, my days were filled with bedside teaching of core pediatric principles and management of pediatric patients in the operating room with anesthesia residents and nurse anesthetists. The hospital provides care for a wide variety of children ranging from an infant with biliary atresia undergoing a Kasai procedure to a healthy eight-year-old with undescended testis. In addition, as a certified Pediatric Advanced Life Support (PALS) instructor, I co-taught a two day PALS course using their well-organized simulation lab and the SimMon app to assist with megacode scenarios.
A few days into my trip the COVID-19 virus began to spread to Africa. Within a day of the first documented case, all the United States university volunteers and Fulbright scholars were asked and then mandated to evacuate and return home. The Rwandan staff were already practicing a ‘no touch’ policy when I arrived, exchanging elbow bumps or foot taps instead of handshakes or hugs, but like most of the world, we did not anticipate how quickly the virus would spread. Although my trip was cut short due to the rapidly spreading COVID-19 virus, I am thankful for my time in Kigali and all the wonderful people I met. I am inspired by their eagerness to learn, ingenuity, warmth, caring, and commitment to service for their country. It was a privilege to work with the anesthesiology staff at CHUK and I would jump at the opportunity to work with them in the future. Thank you Dox Foundation for helping make this trip possible.