We are traveling to Muhimbili University in Dar Es Salaam to begin a women’s imaging fellowship for a large and motivated group of Tanzanian radiologists who are completing residency and beginning subspecialty fellowship. We are beginning this program by introducing the curriculum, teaching image-guided diagnosis and intervention, and helping to protocol patient imaging studies. We will lecture and teach at the workstation both formally and informally. This imaging fellowship will create expertise in the area of women’s imaging to include breast, abdominal, and pelvic benign and malignant diseases. This is an opportunity to advance women’s healthcare in the East African community.
The women of Tanzania. And by proxy, their families. Women of child-bearing age and beyond will achieve benefit from diagnosis and intervention of breast, abdominal, and pelvic diseases, and we will incrementally improve outcomes through image-based diagnosis. By improving diagnostic acumen through imaging, we are able to improve outcomes, to begin to downstage disease, and create awareness of treatable conditions.
Our mission this trip is to begin the specific women’s fellowship training at Muhimbili University. We will be discussing the schedule, the lectures, the curriculum, and the hands-on training. We will be establishing and strengthening critical in person connections. What we begin in Tanzania will carry on remotely and in multiple return trips throughout the trainees’ two year commitment. We use remote calls, WhatsApp and shared learning materials to present and share cases and concepts. A goal is to train a large number of physicians locally using their available resources where effective workarounds may be devised rather than bringing a minority to train at US fellowships.














Tim Rooney, Frank Minja and myself came to Muhimbili University of Health and Allied Sciences (MUHAS) in Dar es Salaam with the intention of developing a Women’s Imaging there. Tim and I are both from the University of Virginia Department of Radiology who practice mammography and body imaging, respectively, and Frank Minja is a neuroradiologist from Emory University. Our group and our RSNA lead on this project, Alice Chong, met with the medical school administration on the still ongoing approval process.
Muhimbili University of Health and Allied Sciences (MUHAS) in Dar es Salaam, is the only university in Tanzania with a 3 year radiology residency in their two teaching hospitals – the Muhimbili National Hospital at its main campus in the heart of Dar es Salaam and the Muhimbili National Hospital Mloganzila on the western end of Dar es Salaam.
As the Radiology residency in Africa is typically a 3 year program after internship, the need for further specialized training was recognized. A collaborative effort (“Road2IR”) between Muhimbili University, Yale Department of Radiology and Biomedical Imaging and Emory Department of Radiology and Imaging Sciences created the first accredited Interventional Radiology (IR) program in East Africa. Frank Minja, MD at Yale School of Medicine, who lived until his college days just outside Dar es Salaam, spearheaded this effort and continues to be part of the interventional Teams of technologists, nurses and physicians from North American Hospitals that come to MUHAS monthly to collaboratively work with the fellows and attendings at Muhimbili. The result is a robust IR training program that has become the destination for IR training for East Africa. The neuroradiology fellowship was begun in 2021. MUHAS currently has partnered with RSNA’s Global Learning Center in September 2020 to focus on additional subspecialty training to include fellowships in women’s imaging fellowship and pediatrics over its 3-year grant period.
One of our goals was also to understand the resources available at the two MUHAS associated teaching hospitals and at a few of the key private hospitals whose association would be expected to mutually benefit a Women’s Imaging Fellowship (specifically Ocean Road Cancer Institute and Aga Khan Hospital). We visited leadership at both these hospitals.
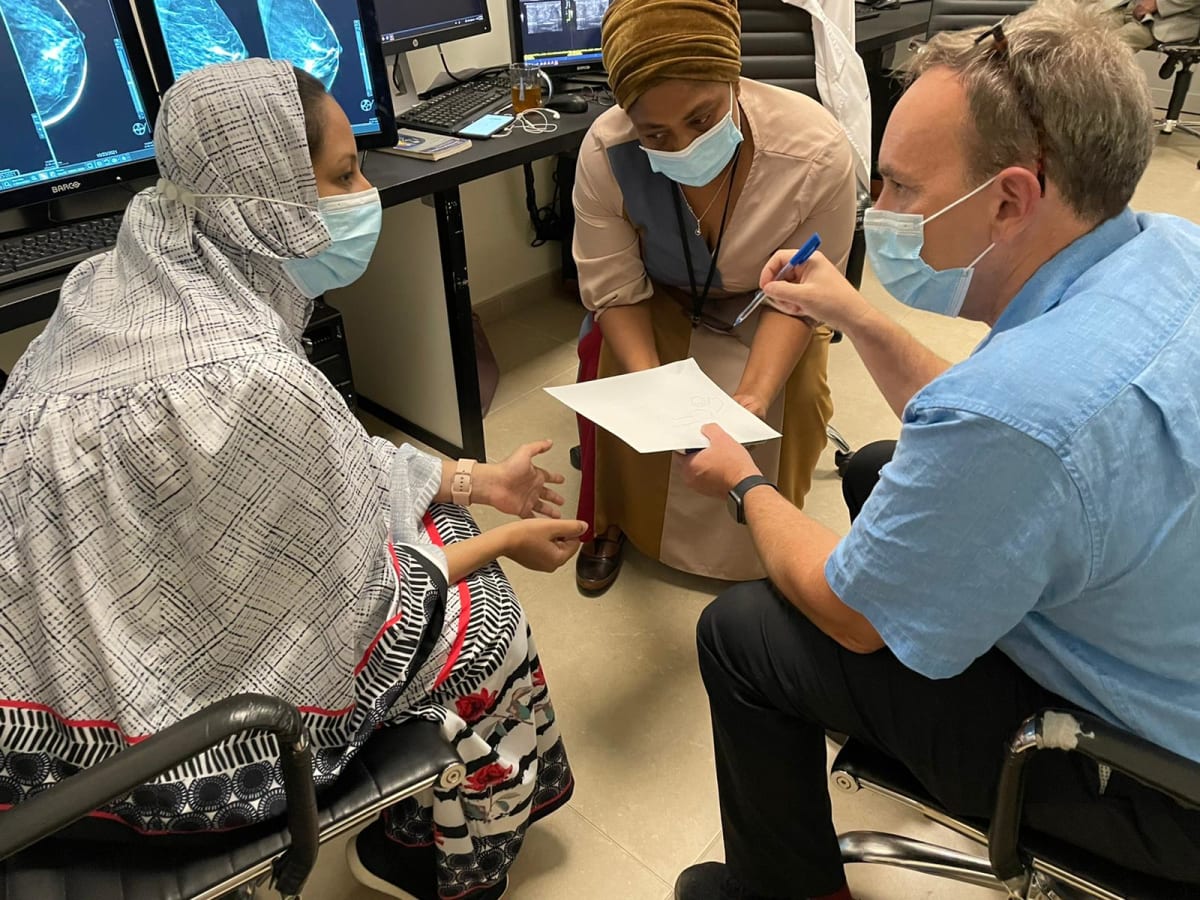
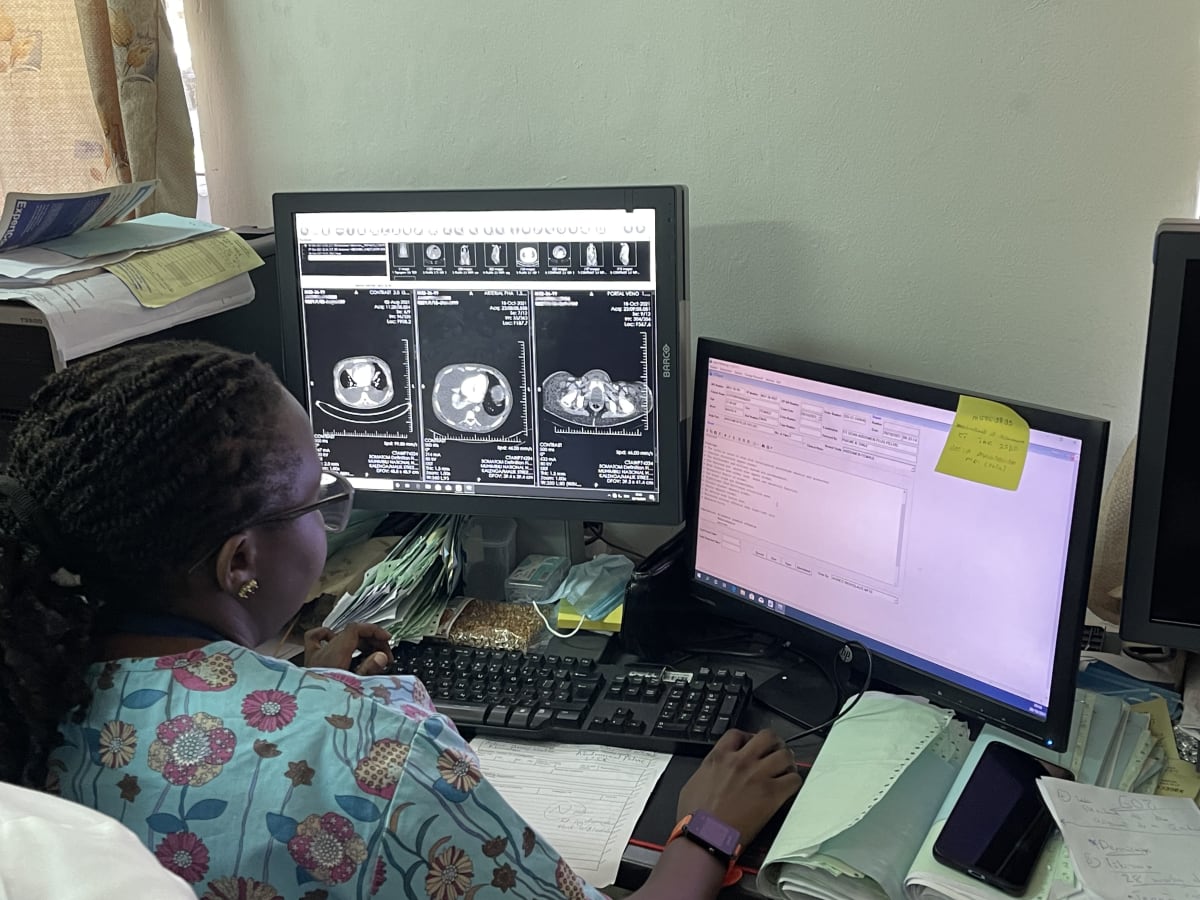
We spent the majority of our time working with the MUHAS attendings. The attendings, who are currently general radiologists, read nearly all studies aside from many of the more complicated neuroradiology studies that are now read by the fellowship trained neuroradiology group. The group is highly interactive, interested, collegial and welcoming. The welcome was incredible to me and something I will always cherish. I was constantly going from one station to another when body imaging and women’s imaging cases came up and we would discuss their cases together. A common discussion we had was over what would the referring physician be looking for.
I spent in particular a lot of time with Drs. Irene Mhalu and Mwejuma Jumbe who are both so smart and engaging and very motivated in seeking this Women’s Imaging Fellowship and are headed towards being movers and shakers in East Africa Radiology. They would need dedicated time from their daily work duties to actually take the role of a fellow to at least participate in interuniversity conferences. Conversely, outside universities with teaching resources available to their own Women’s Imaging Fellowships would ideally need to provide or participate in these shared conferences. The existing imaging equipment may need servicing or upgrades. We saw a modern mammography unit at MUHAS waiting to be installed. Other hospitals associated with this fellowship may be able to provide imaging when a void exists. We learned that the need for robust service contracts in addition to equipment acquisition cannot be overemphasized. We noted that MUHAS has a new 3T Siemens MRI and are anxious to use it for breast MRI. A benefit from the fellowship is perform breast MRIs in more appropriate and tailored treatment algorithms.
The Women’s Fellowship curriculum would at least be inclusive of breast and pelvic imaging. This curriculum development is an ongoing work in progress. The success of the neuroradiology and IR programs is a great predictor of the likelihood of success of a women’s imaging program. Specialization will result in greater collaboration with disease specific referrers and imaging and reporting will be more appropriately tailored to the current clinical practice. Referrers may include at least include those in breast and gynecologic surgery, oncology and radiation therapy. We were very aware of the need for this subspeciality training for result in the kind of collaboration needed for optimal diagnosis and treatment.
Having easy access to clinical history and frequent dialog with the referrers directly or in tumor boards is a work in progress. This will continue to evolve with further improvements in the infrastructure. RSNA has given the university a grant for high speed internet and access to all RSNA related journals, on line conferences and other RSNA resources. An ongoing need is for a readily accessible electronic medical system and a radiology information system to supplement their open source ClearCanvas PACS system.
Aside from administrative meetings in offices, we often extended these meetings out at dinner which continued the effort of developing a program. Making and maintaining these personal contacts particularly goes a long way in achieving a goal. Doximity’s Dox Foundation funded our plane tickets and remained a personally accessible organization to whom we are deeply grateful.