My time in Blantyre, Malawi will be spent serving at Queen Elizabeth Central Hospital - (known as the AETC- Accident and Emergency Trauma Center). This facility is one of the only emergency/trauma centers in the country and often is responsible for care of those traveling through remote regions of surrounding countries. Through my residency program I am blessed to have a close connection with Dr. Carly Brady, who was fundamental in the development and continuation of the emergency medicine training program in Blantyre. I recall one specific story she tells about a polytrauma after a minibus accident. The patients were quickly stabilized in Zambia and then transported (by another minibus!) to the hospital in Blantyre, 14 hours away! On arrival, it was realized the ‘stabilization’ consisted of a total of SEVEN right arm amputations. The remaining patients had a mix of other acute injuries all requiring urgent attention. It is nearly impossible to fathom this degree of need that those in remote regions of the world experience. I am both excited and terrified to join the crew at Queen Elizebeth’s for a month this Fall.
Specifically, I will be working alongside Dr. Brady, other EM faculty, and the emergency medicine residents at Queen Elizabeth, joining them in learning and seeing and treating patients. I am especially excited to gain further insight into medical decision making with limited resources. I feel that this experience will especially help me hone in on my physical exam skills and differentiating between the fine line of ‘sick vs not sick’. In a country with less than a hand full of CT scanners, you need to be sure when asking for imaging!
I have had a passion for palliative care in the global setting for some time. Through our connections with the residency program in Malawi, I have been able to get in contact with their director of palliative care. During this rotation, I hope to explore the possibility of introducing palliative into the emergency set
The population that will be benefiting from this trip is multifold. Directly and most specifically, I aim to serve the people of Malawi and surrounding regions who rely on Queen Elizabeth for healthcare, as it is one of the only centers of its kind in a ‘health care desert’. On a broader scale, I hope to learn with and assist in the teaching of my temporary co-workers in the hospital, with simulation based training and didactics.
Global health exposure, on any scale, is a valuable experience to health care learners as it provides unique experiences, a wide range of pathologies, and a deeper understanding of humanism. The rotation at Queen Elizabeth specifically is a very special opportunity granted to residents as it takes place at one of the leading academic institutions in Africa. Rotators learn in a supervised environment and are exposed to a wide breadth of pathology not encountered in the United States. The emergency department is well developed with its own trainees, and has access to many of the modern technologies available at Prisma, but on a much more limited scale. This requires special attention to history and physical exam skills in order to preserve resources, something that is not as heavily considered in the Western world. It will also be interesting to consider alternative treatments to diseases that I am already familiar with, not to mention the new conditions that I am sure to gain exposure to while working in a foriegn environment. I am also excited to broaden my knowledge on health care systems around the globe. Lastly, and probably most importantly, the shift in perspective I always experience upon completing a global health trip is very humbling. I hope to return from this rotation with renewed patience, gratitude and motivational drive to improve health care access to my own future patients.
















I love the term “well wishers” as opposed to bystanders. Bystanders are passive perhaps with an illusion of concern. Well wishers engage and act with a purpose to help. On a routine day at Queen Elizabeth Central Hospital (Queens), a middle-aged man who had the misfortune of being hit by a car was brought to the Accident Emergency and Trauma Center (AETC) by “well wishers”. These accidents are not uncommon in the crowded streets surrounding Blantyre. Well wishers had taken it upon themselves to assist this stranger with the hope his life could be saved. Bystanders had gone about the business of the day after saying ‘someone should do something’.
This patient’s Glasgow Coma Scale was 6, where any score less than 8 represents a serious brain injury. On American soil, this man would have been intubated immediately. Not here. During my time at the hospital, I didn’t see a single patient undergo rapid sequence intubation, though there had been countless deserving of it. What would we do? Bag them all day? There was an ICU on the grounds though. But it was Understaffed. Under-equipped. And should the man recover enough to be transferred out of the ICU? What then? Trach? Peg? Months of rehab? Not in Malawi. Though no information was known about this patient, we set about practicing medicine as best we could. Surprisingly, Queens Hospital does have a CT scanner, though the process of obtaining a CT scan is rigorous. But our patient needed one. Later, I would think to myself, “Why scan this patient?” Though there is a neuro ICU with bolt capabilities at Queens, it sometimes seems hopeless. The same sequence flashed across my mind.. Trach. Peg. Rehab.. Family members unable to support him.. But there is always hope. When it was this patient’s turn to go to the CT scanner. My attending and I looked around the overcrowded resus bay to catch the eye of one of the nurses to help with transport. When no help was offered, Dr. Brown grabbed the beat-up transport box and off we went, dragging the creaking bed through the swinging doors. The bed our patient inhabited was one with a modern, lighter frame as opposed to the iron, practically immovable styles of most patients. Much more maneuverable. This came at the expense of safety as there was only one flimsy guard rail corralling our patient who was just active enough to pose a true risk of falling. Queens was built in pieces. Think of one of those green Lego bases with houses made of classic bricks strewn chaotically. The corridors are framed with windows that have low hanging ceilings and concrete floors. It had, of course, been raining that day leaving a slick film of mud over the concrete. Thankfully, there was no standing water. We wheeled our patient into a bit of a holding room to wait our turn for CT. At one point, I looked down and noticed a black plastic bag tucked between our patient’s shoulder and neck. I fought back the tears as I made out its contents: a loaf of bread and some juice. Our patient was just trying to buy groceries and the luck of the world landed him here. The radiology attendant’s voice snapped me from my contemplation. We wheeled him into the next room and safely maneuvered his uncooperative body over to the CT scanner. After strapping him in, we waded into the viewing room. Our faces turned grim as the evidence of a large epidural head bleed flickered across the screen. Solemnly, we transferred the patient back to the stretcher and started the trek back to the AETC. Much of the route to radiology is downhill which presents its own perils. The trip back, however, is uphill and is topped off with a gradient that defies all ADA requirements. We rounded the corner, security guard shuffling a gate out of our way, and began to pump our legs to gain the momentum we would need to get our patient up the steep grade. Surprising even myself, I started laughing…out loud…just over the irony and idiocy of it all. I could not help but grin madly. I felt insane. Though we had started at a sprint, our pace had slowed dramatically due to the steepness just before the summit. Out of breath, we finally heaved through the threshold and into the AETC.
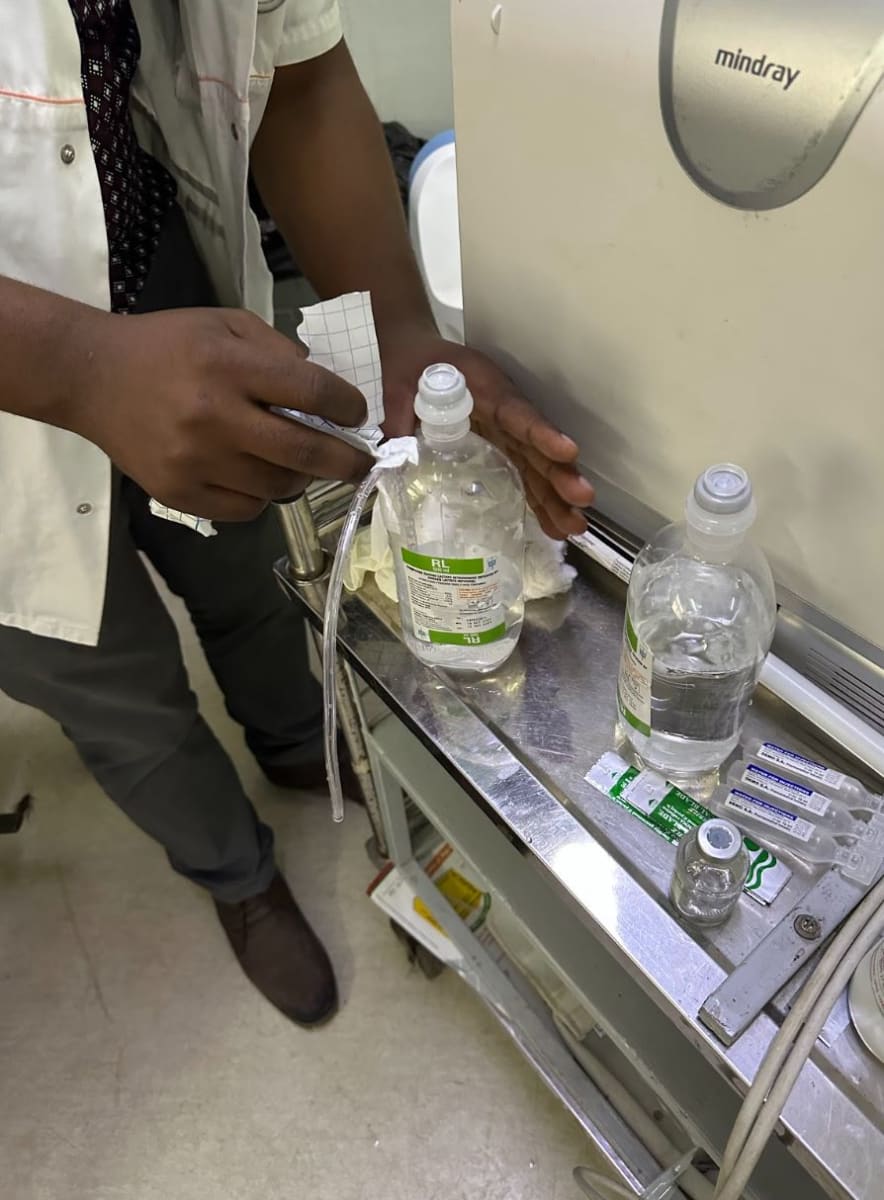
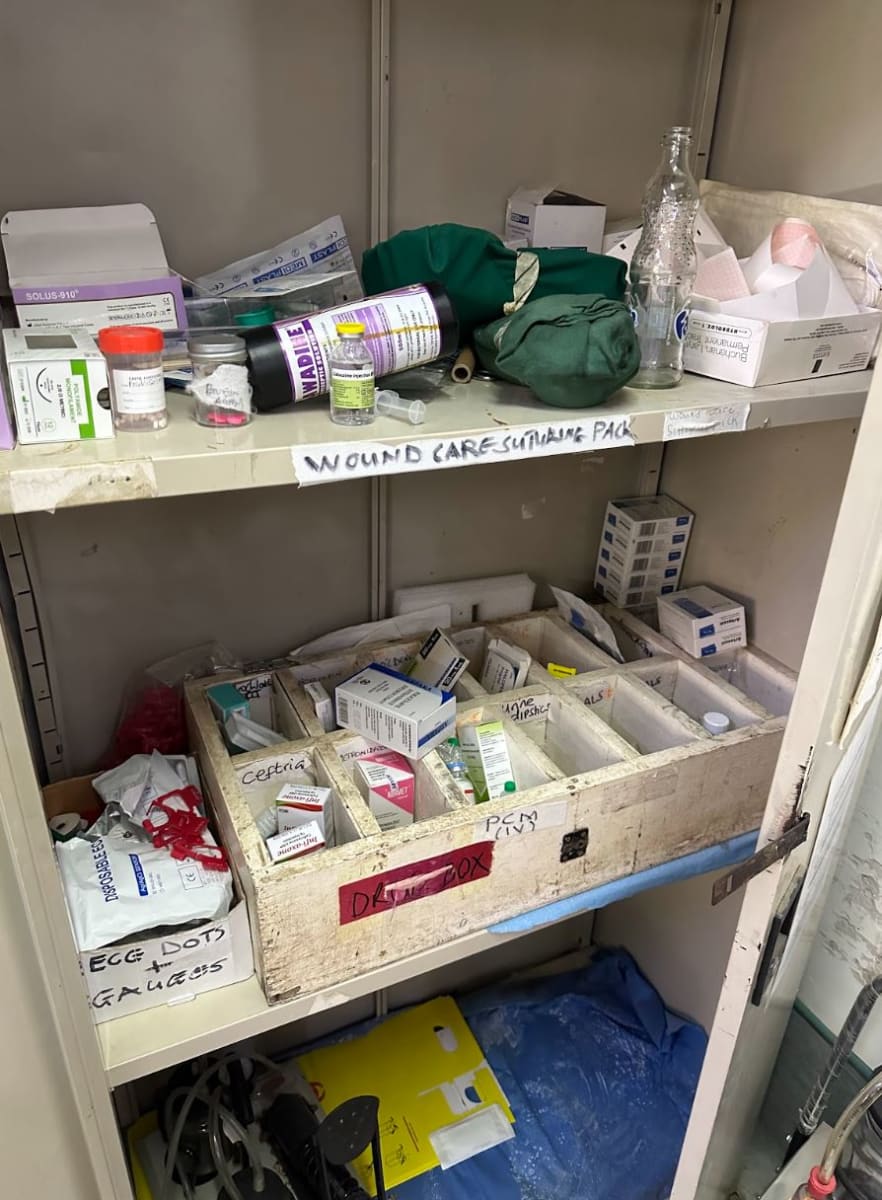
The burden of disease here is unfathomable. I remember Dr. Caroline Brady, the Head of the Emergency Medicine Unit, recounting some of her biggest frustrations to me. “It isn’t always that we don’t have the resources to take care of people; It’s also that they come to the hospital extremely late into the clinical course!” I can specifically remember one 15 year old male patient who was held at a district hospital for several days with a worsening intracranial abscess. As for resources.. Antibiotics? Two. Rocephin and Flagyl. Lots of Versed. Queens uses aminophylline for severe asthma exacerbations. We made our own Pleur Evacs and there is no such thing as a lumbar puncture “kit”. They usually have bicarb, at least in the central pharmacy if not in the ‘emergency trolley’ (crash cart). There is even epinephrine, which is exclusively referred to as adrenaline. There is usually an ample supply of IV fluids, of course, until there isn’t. And then a cholera patient dies of dehydration.
Dr. Brady continued the conversation a week later over dinner, “It’s literally like you are playing God some days deciding who will live and die simply by allocation of resources.” But really, it is the patients who should have come to the hospital a week ago or the ones who festered in packed wards at a district hospital before being transferred that will haunt you. Patients who might have had a fighting chance in the early stage of their disease but now, unfortunately, have become a lost cause. Transportation issues, inability to miss work, fear of cultural repercussions…just some of the reasons care is delayed. There was a survey discussed at a local Research Dissemination Seminar polling mothers on why they did not bring their children to pediatrics appointments. Most of the mothers’ responses correlated with “laziness”. Even in a world where the daily toil consumes the effort of a week’s worth of work stateside, mothers described themselves as lazy. Unbelievable. In Blantyre, I witnessed levels of hardship and poverty to the extent I had never seen, or even imagined, before. And the bearers of these lives who worked so hard just to survive considered themselves lazy? And even worse, I knew the experiences I was exposed to were just the tip of a systemic injustice iceberg. I am both humbled and motivated by my experiences in Malawi, where I experienced first hand how inequity translates into the practice of Emergency Medicine. I can’t imagine how it is not everyone’s life goal to be a “well wisher” and act to level the disparity. My time at Queens has reinforced my desire to encourage both myself and others to reject the notion of being a bystander and to join in being well wishers to society.